Other Treatment Methods
.webp)
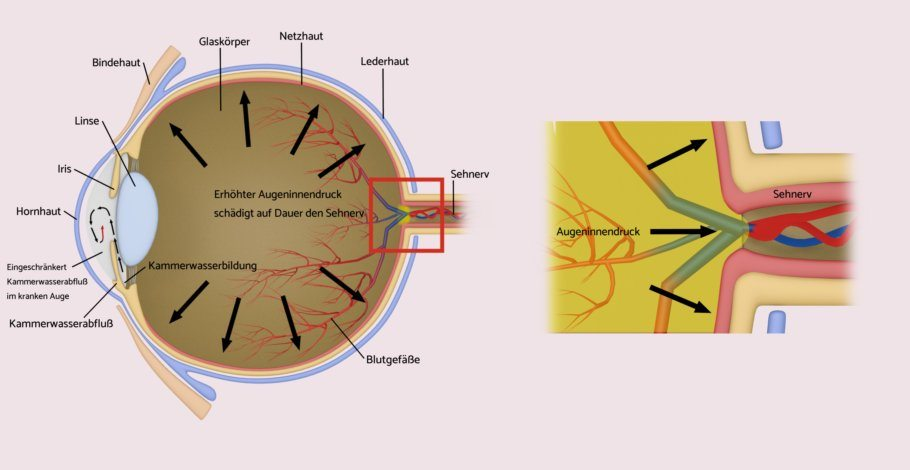
Green star (glaucoma)
Doctors have known about glaucoma, also called glaucoma by professionals, for about 150 years. Here, increased intraocular pressure damages the optic nerve with its highly sensitive nerve fibers, which transmit the impulses of the photoreceptors into the brain (visual cortex). As a result, the field of vision gradually narrows until those affected become completely blind.
To this day, glaucoma is considered the second most common cause of total vision loss. Initially, those affected do not notice this loss of visual field because the gaps are compensated by the brain and nerve fiber loss is completely painless. Intraocular pressure is regulated by the aqueous humor and is additionally influenced by blood pressure and the general vascular condition. In nine out of ten cases – primarily in older age – an open-angle glaucoma occurs, in which the outflow obstruction is directly in the outflow area of the eye angle.
The narrow-angle glaucoma
Another common form of glaucoma is the so-called narrow-angle glaucoma. It predominantly affects far-sighted people. In their case, the chamber angle is too narrow due to the shorter eye (Far-sightedness), so that the aqueous humor drains insufficiently. These individuals are also at risk of an acute glaucoma attack. In this situation, the chamber angle is suddenly completely blocked and the intraocular pressure rises abruptly. Affected individuals complain of severe pain, deteriorating vision, nausea and vomiting. In this medical emergency, the ophthalmologist must act immediately, as otherwise the optic nerve will be irreparably damaged.
Aqueous humor is continuously produced by the so-called ciliary body. This ring-shaped structure is located behind the iris (the colored part of the eye) and is not visible from the outside. The crystal-clear aqueous humor is constantly exchanged and flows from the eye toward the chamber angle. Here, the aqueous humor first passes through the trabecular meshwork, a dense lattice that acts as a type of filter. Behind it lies Schlemm's canal, which drains the aqueous humor into special veins. The normal intraocular pressure averages 15 mmHg. At this value, there is a balance between production and drainage.
Diagnosis of glaucoma
The most important instrument is the computerized measurement of the optic nerve head. Furthermore, all eye sections are examined microscopically and the intraocular pressure is measured. Depending on the condition of the optic nerve head, the doctor can determine whether there is a suspicion of glaucoma. If this is the case, the ophthalmologist can resort to further useful diagnostic methods such as the measurement of the visual field and the nerve fiber layer.
Treatment options for glaucoma
First, the ophthalmologist tries to lower the intraocular pressure with eye drops. If successful, the patient will now undergo close follow-up checks with eye pressure, visual field, and nerve fiber layer measurements. In addition, he usually has to use drops for life. A cure for glaucoma is not possible. If the medication is not sufficient, several surgical treatment methods are available. They either improve the outflow or reduce the production of aqueous humor. The procedure is performed using laser or scalpel.
Laser therapies for glaucoma
YAG iridotomy – prevention of an acute glaucoma attack (angle-closure glaucoma)
Procedure: outpatient, local anesthesia with eye drops, patient sits at the microscope
Farsighted patients have an increased risk of an acute glaucoma attack. The ophthalmologist can assess such a risk during the microscopic examination based on the anatomical situation of the eye. Depending on the situation, he will recommend a special laser treatment that can prevent such an attack. For this purpose, a small hole is created in the iris with the laser so that the aqueous humor can circulate again.
Improvement of outflow (ALT/SLT)
Procedure: outpatient, local anesthesia with eye drops, patient sits at the microscope
In this procedure, the doctor treats the trabecular meshwork with very short and very small laser pulses. As a result, the meshwork expands, and the aqueous humor flows out more easily. The intraocular pressure decreases by 6 to 8 units (mmHg). After 4 to 6 weeks, the maximum therapeutic outcome is achieved. The treatment can be repeated and is effective for up to two years. However, it does not help all patients.
Inhibition of production (CPC)
Procedure: outpatient, local anesthesia with injection next to the eye, in the operating room
In this laser treatment for glaucoma, the ophthalmologist uses laser pulses to cauterize parts of the ciliary body. The ciliary body produces less aqueous humor, and the intraocular pressure decreases. Three months after therapy, the maximum effect of the therapy is reached. During this procedure, the ophthalmologist must be very careful not to cauterize too much tissue, as this would result in too little aqueous humor being produced. He may, therefore, need to approach the individually necessary dose in several sessions. Occasionally, the doctor also uses a cryoprobe for the procedure (so-called cyclophotocoagulation).
Implants for glaucoma
Improved drainage with iStent inject®
Procedure: outpatient, local anesthesia with eye drops
Implants have also made their way into ophthalmology, which, similar to vascular and cardiac surgery, restore or improve flow. The iStent® is particularly suitable for patients with glaucoma or cataracts suffer. Here, during cataract surgery, the doctor can implant an iStent® into the chamber angle (specifically: into Schlemm’s canal) with low risk. The iStent® is the smallest known implant in the human body. It is made of non-magnetic titanium. Up to 3 out of 4 patients require no further therapy after the operation, or only need pressure-reducing eye drops.
Canaloplasty
Improved drainage by dilating the natural canal
Procedure: outpatient under general anesthesia or with local anesthesia via injection next to the eye, in the operating room
In this new micro-invasive procedure, Schlemm’s canal is probed using a microcatheter and dilated along its entire length with a tensioning suture. The demanding intervention is very low-risk and achieves medium- to long-term pressure reduction.
Surgery for Glaucoma
Improved drainage through surgically created canal
Procedure: outpatient, local anesthesia via injection next to the eye, in the operating room
This glaucoma operation is among the most proven but also most invasive techniques. It is the last resort in surgical options and has the strongest pressure-reducing effect. In this procedure, the eye surgeon creates a channel from the chamber angle through the sclera of the eye to beneath the conjunctiva. This creates a filtering bleb below the upper eyelid. After the operation the patient will be closely monitored until the intraocular pressure has stabilized. Risks are an excessive reduction in pressure shortly after the operation and a blockage of the canal due to the healing process.
Summary
Glaucoma is one of the few diseases that can be detected and treated early through preventive examinations. The goal of therapy is to optimally adjust intraocular pressure in order to slow down the progressive damage to the optic nerve head as much as possible, and to preserve the visual field as comprehensively as possible. However, the doctor cannot reverse any existing damage. He does, however, have numerous highly precise diagnostic options at his disposal to monitor the course and to offer an individualized therapy in a timely manner.
Experts for this Treatment Method

- Modern Ophthalmology
Dr. Mirka R. Höltzermann
Augenpraxis Dr. Höltzermann, Dr. von Schnakenburg, Augenpraxis Dres. Höltzermann & von Schnakenburg
- Modern Ophthalmology
Dr. med. Ilya Kotomin
Smile Eyes Leipzig
- Modern Ophthalmology
Priv.-Doz. Dr. med. Daniel Pilger
Smile Eyes Berlin
- Modern Ophthalmology
Raphael Neuhann (FEBO)
Opthalmologikum Dr. Neuhann / Augentagesklinik am Marienplatz
- Modern Ophthalmology
Dr. med. Tabitha Neuhann
Opthalmologikum Dr. Neuhann / Augentagesklinik am Marienplatz
- Modern Ophthalmology
Prof. Dr. med. Tanja M. Radsilber
Augenzentrum Prof. Dr. med. Holzer & Prof. Dr. med. RabsilberAll Experts in this Department
Show All
- Modern Ophthalmology
Dr. Mirka R. Höltzermann
Augenpraxis Dr. Höltzermann, Dr. von Schnakenburg, Augenpraxis Dres. Höltzermann & von Schnakenburg
- Modern Ophthalmology
Dr. med. Ilya Kotomin
Smile Eyes Leipzig
- Modern Ophthalmology
Priv.-Doz. Dr. med. Daniel Pilger
Smile Eyes Berlin
- Modern Ophthalmology
Raphael Neuhann (FEBO)
Opthalmologikum Dr. Neuhann / Augentagesklinik am Marienplatz
- Modern Ophthalmology
Dr. med. Tabitha Neuhann
Opthalmologikum Dr. Neuhann / Augentagesklinik am Marienplatz
- Modern Ophthalmology