When toe and chair leg meet, pain is a pretty clear thing. But what if the pain cannot be precisely attributed? And that over the years? Is it just imagined, as many say? However, around 12 million people in Germany are affected by it.
According to the German Pain Society , costs of about 38 billion euros arise annually - 10 billion of which are for treatments, while the rest is caused by sick pay, work absences, and early retirement.
New approaches to dealing with chronic pain
Dr. Claudius Gall, a specialist in neurosurgery, is one of the few specialists in Germany in this field with the additional designation "Special Pain Therapy." In the "Pain Workshop" in Munich, he and his colleagues deal with the backgrounds and new approaches to dealing with chronic pain.
What exactly is pain?
Pain is initially a "perception." This means every pain is real – there is no imagined pain. The body is supplied with pain fibers everywhere except the brain. If these are stimulated – by whatever means – it leads to pain. However, there are two different mechanisms that lead to the sensation of pain: acute and chronic.
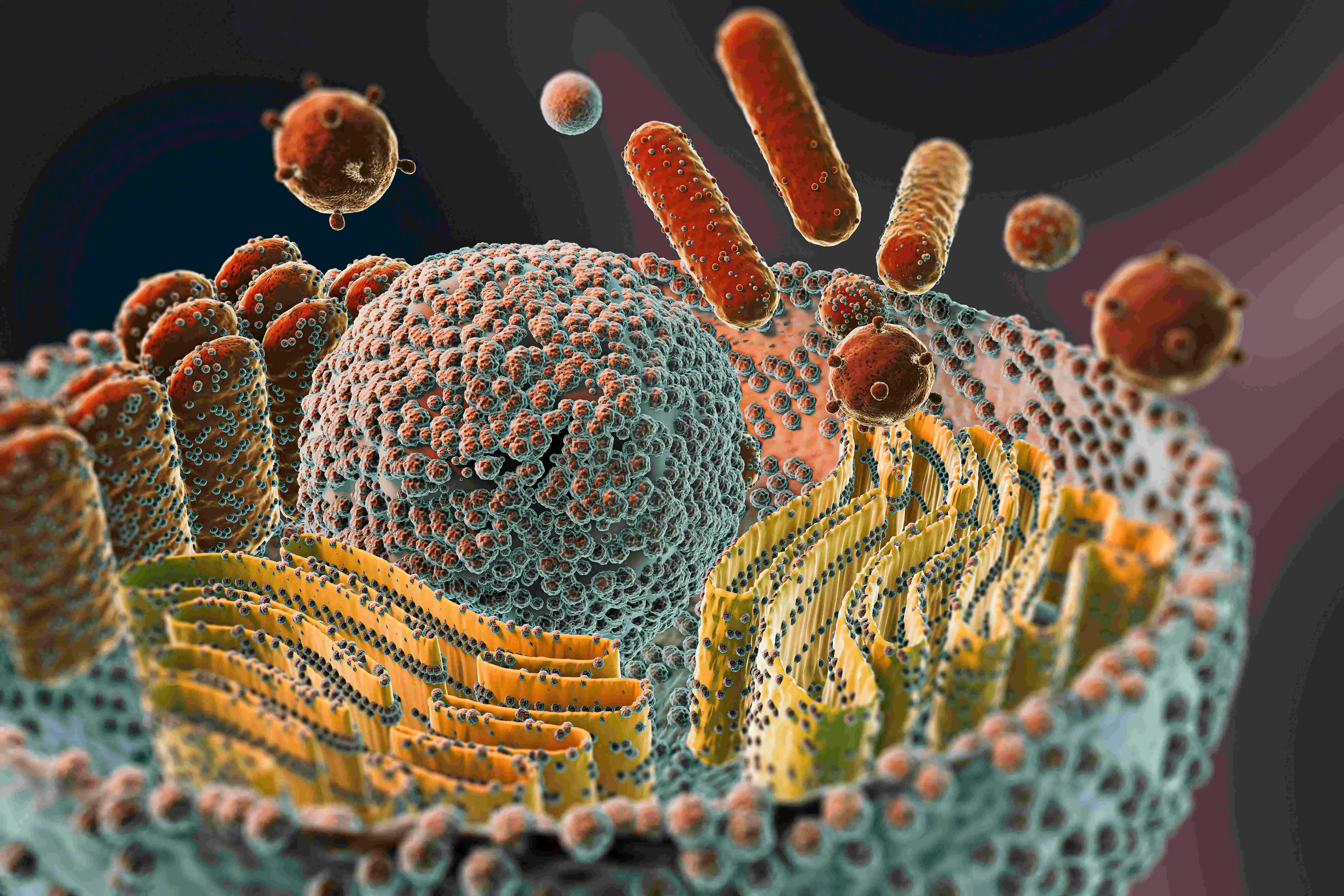
What's the difference?Acute means: hand on a hot stove. Tissue destruction releases electrical impulses that travel via the spinal cord to the brain and into consciousness. Chronic pain arises from a malfunction of certain nerves and can develop as a result of an acute pain experience.
A classic example is phantom pain, such as pain in a non-existent knee joint during weather changes.
How can chronic pain be recognized?
This is pain that lasts longer than 6 months in the same region and has at least a moderate intensity. Chronic pain also leads to side effects in all areas: it affects the sleep-wake cycle, mood, and libido.
Thus, chronic pain becomes an independent condition – it has physical elements at the nerve cell level but also interferes with many other social, private, and professional areas. Our task in pain therapy is to find out the relationship between acute and chronic pain, as both must be treated very differently.