The dangerous alliance of two proteins
Sometimes it is not what is missing, but what is wrongly connected. A new study by Rockefeller University shows that two proteins – amyloid-beta and fibrinogen – together have a devastating effect on the brain. In tiny amounts, which would be harmless on their own, they jointly lead to massive neuronal damage – and significantly accelerate Alzheimer’s processes.
This insight not only adds a new piece to the complex puzzle of the disease, but also new hope for therapies that intervene early – long before memory loss and cognitive failures become visible.
When amyloid meets fibrinogen
Amyloid-beta (Aβ) and tau proteins have been considered the central ‘suspects’ in Alzheimer’s research for decades. But the simple formula ‘too much amyloid – equals Alzheimer’s’ falls short. Researchers around Prof. Sidney Strickland and Dr. Erin Norris now show that amyloid-beta 42, the particularly toxic variant of the peptide, forms a dangerous alliance with another protein: fibrinogen.
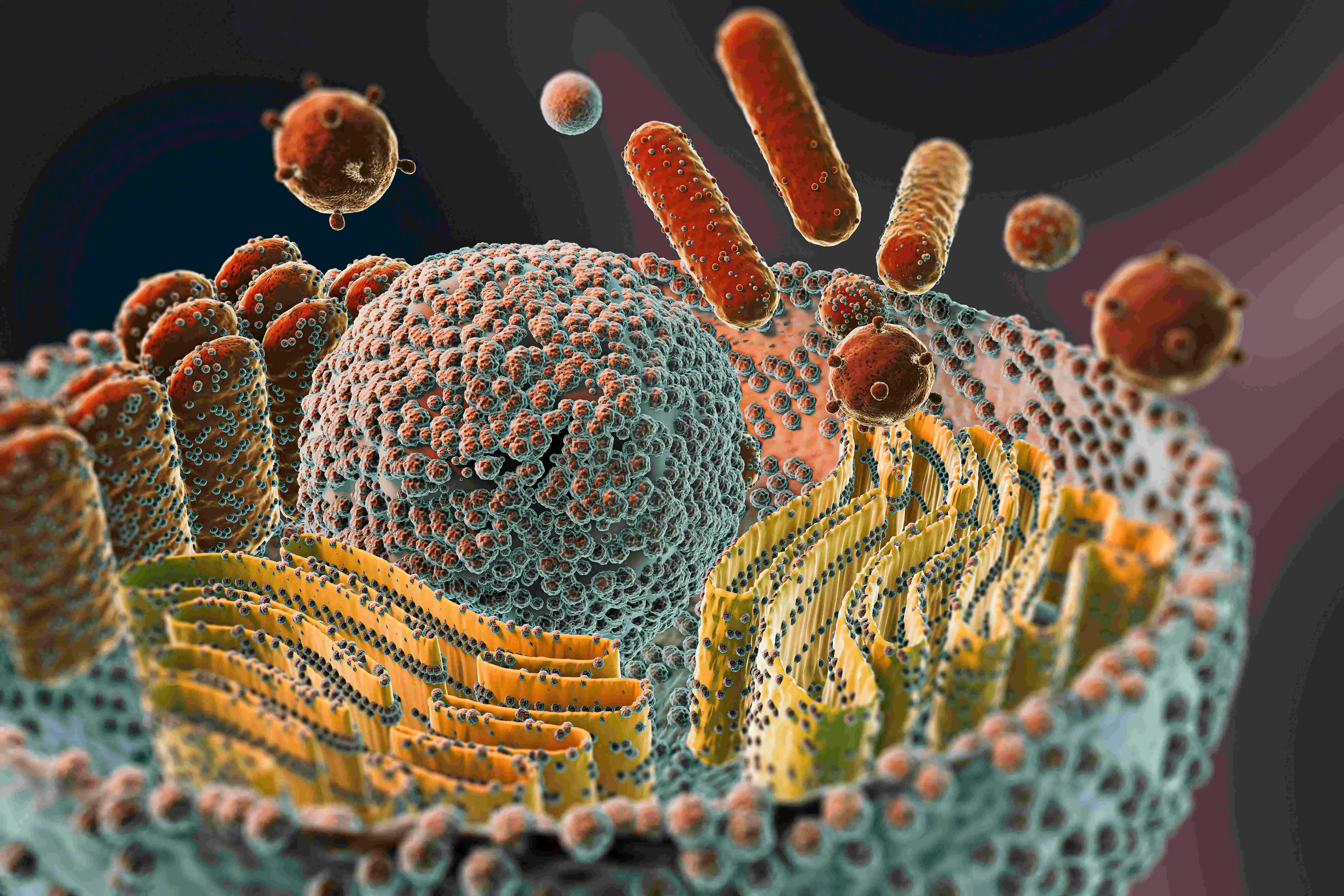
Fibrinogen is actually a harmless component of blood. It ensures blood clotting by being converted into fibrin in case of injuries – a kind of body’s own plaster. However, it should not be present in the brain. Only when the blood-brain barrier, that delicate protective barrier between the circulatory system and nerve cells, becomes permeable – as often happens in the course of Alzheimer’s – does fibrinogen enter brain tissue. There it meets amyloid-beta. And this encounter has fatal consequences.
Small amounts, big impact
To investigate the effect, the researchers relied on a sophisticated model: They used tiny slices from the hippocampus of mice – the area where memories are formed. These ‘organotypic brain slices’ stayed alive and responded to the addition of various protein mixtures.
The result was astonishing: Neither amyloid-beta nor fibrinogen alone caused visible damage at low concentrations. However, as soon as both molecules acted together as a complex, synaptic markers—the metric for healthy neuronal communication—collapsed massively. Even tiny amounts of the duo led to the same damage as high doses of amyloid alone.