Other Treatment Methods

Keratoconus
Keratoconus is a progressive thinning and bulging of the cornea of the eye (cornea) associated with fluctuating and decreasing visual acuity. Keratoconus is also one of the most common reasons for a corneal transplant. The earlier it is detected and stabilized, the greater the chance of preventing it.
Keratoconus is a non-inflammatory disease of the cornea of the eye, where it thins and bulges further until it takes on a conical shape. The bulging often occurs in the lower part of the eye. Around one in 2,000 people is affected – typically at both eyes but at different times. Keratoconus usually occurs in the second to third decade of life and comes to a halt between the fourth and fifth decade. In some patients, the progressive form of keratoconus can not only make wearing special contact lenses impossible but also require a corneal transplant.
Diagnosis of keratoconus
In the early stages, this rare eye disease often confused with irregular astigmatism and not yet recognized. Therefore, it is important to accurately diagnose keratoconus through an examination of the corneal surface and back, corneal thickness, and possibly an endothelial cell count. Keratoconus is likely a disorder involving the collagen molecules of the corneal connective tissue scaffold, leading to reduced collagen cross-linking and thus decreased biomechanical stability. The causes are complex and not yet fully understood. Genetic predisposition is suggested by its frequent familial occurrence. Therefore, genetic testing and counseling are recommended in the context of future family planning. Immunological factors may also play a role. However, it is only certain so far that vigorous and frequent eye rubbing over years, for example, in allergy sufferers, represents a high risk factor for developing keratoconus.
Symptoms of keratoconus
Possible consequences of keratoconus are unusual fluctuations and decrease in visual acuity, irregular astigmatism, perception of light rings around light sources, known as ‘halos’, as well as increased light sensitivity and glare. If the disease remains in a stage where the full cone shape has not yet developed, it is called ‘keratoconus forme fruste’. However, 20% of patients develop progressive keratoconus, which usually progresses progressively and requires surgical intervention (cross-linking, intracorneal ring segments (ICRS), DALK). This can lead to tears in the posterior corneal membrane – rupture of Descemet’s membrane – causing fluid from the anterior chamber to enter the cornea and make it cloudy. This is then referred to as acute keratoconus. In the late stage, only a corneal transplant helped.
Treatment of keratoconus
The therapy of even advanced keratoconus is currently undergoing intense change. The use of the Bowman’s membrane of a donor cornea as an implant can be helpful, as well as recently the implantation of semicircular segments of a donor cornea or ring segments made of synthetic material (Intacs).
Another interesting new development for the treatment of keratoconus, especially if corneal transplantation is to be postponed, is the Xenia® implant. Made from natural corneal collagen, alien cells are decellularized to create a highly compatible implant with no blood vessels or nerve fibers. The manufacturing process is reminiscent of the development of biological heart valves.
Further information can be found at: https://xenia-implant.com/
Crosslinking (CXL)
After local anesthesia with eye drops, the sealing layer of the cornea, the epithelium, is carefully removed because riboflavin (vitamin B2 eye drops) does not penetrate the epithelium. Subsequently, riboflavin is dripped onto the cornea until it is well soaked. Finally, the cornea is exposed to UV-A light for 5 minutes. At the end of the operation, a bandage contact lens is placed on the cornea: This remains on the eye for a few days until the epithelium has regenerated.
Iontophoresis Crosslinking
The term "iontophoresis" is composed of the word 'ion' and the ancient Greek word pherein 'to carry' and refers to a method by which drugs are transported through the skin with the help of slightly electrically charged ions. In this case, the active ingredient riboflavin (vitamin B2) is transported through the corneal epithelium into the deeper corneal stroma so that it can take effect there. Iontophoresis crosslinking is therefore one of the procedures also known as transepithelial crosslinking (TE-CXL).
Vision correction with the help of contact lenses
By wearing glasses or contact lenses, astigmatism and myopia can be corrected after stabilization of the cornea has been achieved. Alternatively, contact lenses can also be implanted (EVO Visian ICL).
Intracorneal Ring Segments (ICRS)
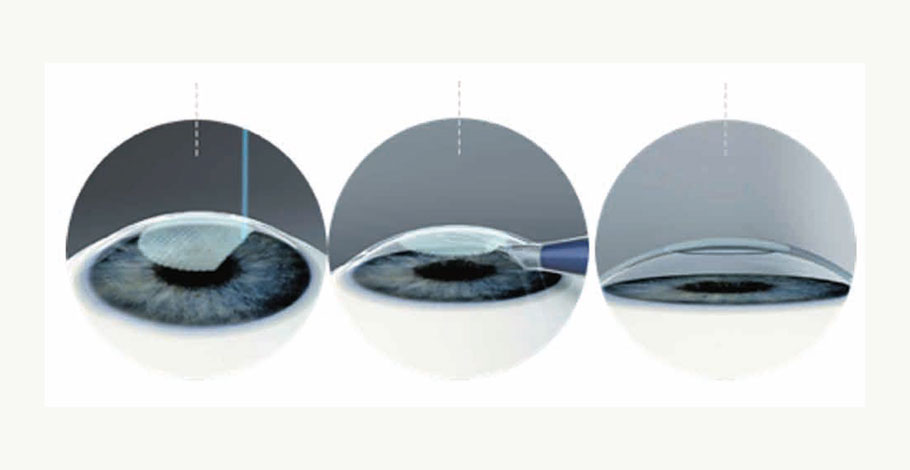
Intracorneal ring segments (ICRS) are two small ring halves that are implanted in the cornea about a year after an initial stabilizing treatment of keratoconus or simultaneously. The ring segments stabilize and flatten the central cornea and can thus also correct myopia. They are made of polymethyl methacrylate (PMMA), which has been used for decades to make intraocular lenses (IOLs). Using a femtosecond laser, a tunnel is first prepared into which the ring segments are carefully inserted. This technique is gentler than manual implantation. Depending on the findings, consideration can then be given to inserting an implantable contact lens to improve visual quality.
The MyoRing
The MyoRing is a closed ring that is inserted 0.3 mm below the surface into the cornea. There, it takes on two functions: it flattens the cornea, which is protruded by keratoconus, and stabilizes the tissue by evenly distributing the pressure exerted on the cornea from the inside. This can slow down or even stop the progression of keratoconus.
The XENIA® Implant
The implant is made from natural collagen of the pig cornea, which is very similar to the human cornea. In a very special process, foreign cells and antigens are completely removed, known as decellularization. The same process has been used for over 30 years for the manufacturing of biological heart valves. It is therefore better than a human transplant because the latter always contains foreign cells from the donor. Another special feature is that each Xenia® implant is individually manufactured according to the anatomical corneal findings. Further details about the implant, manufacturing, functionality, and literature can be found at https://xenia-implant.com.
In summary, keratoconus is a disease where proper and early diagnosis is particularly important. Highly fluctuating values of astigmatism and myopia should alert the attending eye doctor. With the right diagnosis, there are successful treatment options with the prophylaxis of 'not rubbing the eyes', crosslinking, gentle iontophoresis crosslinking, ring segments, and recently with the individually adapted XENIA® implant to stop the progression of the disease and initially avoid a corneal transplant. Unfortunately, this is still not successful in all cases. The latest publications suggest that keratoconus is a bilateral disease and therefore requires prophylactic bilateral therapy.
Forms of Keratoconus
Forme Fruste
The forme fruste is indistinguishable from normal corneal astigmatism in terms of its symptoms and is often discovered incidentally during a thorough ophthalmological examination. It can be corrected with glasses or contact lenses and does not need treatment if stable, but should be monitored and regularly checked. The forme fruste is ten times more common than the progressive form. As a prophylactic measure, it is strongly recommended not to rub the eyes with the hand.
Progressive form of keratoconus
The progressive form of keratoconus is aggressive and often becomes noticeable in the teenage years. The progressing bulging causes corneal astigmatism. Due to this irregularity of the cornea, correction with glasses becomes increasingly difficult. Contact lenses are more suitable as they exert pressure on the cornea and can correct the most severe irregularities. If the disease has not progressed too far, a good correction can be achieved with lenses, up to maximum visual acuity. However, if the corneal protrusion continues to increase, even hard contact lenses fit less stably and can fall out. Additionally, with the progressive protrusion, the cornea below the center becomes increasingly thin and scarred, irreversibly impairing sharpness of vision. The treatment principle is strictly based on the safety of a treatment and evidence-based medical findings. Based on the diagnosis, the following therapies are available in this order. In the first step, the progression of the disease is curbed, and in the second step, vision correction is pursued.
1. Stop the progression of keratoconus
• It is strongly recommended not to rub the eyes.
• UV Riboflavin Crosslinking (CXL)
• Gentle CXL in the form of iontophoresis crosslinking (ICXL)
2. Improve visual quality
• Vision correction with contact lenses of any kind:
• soft-, rigid- contact lenses or scleral shells
• If contact lenses are not tolerated, implantable contact lenses can also be used
• Implantation of intracorneal ring segments or
• Implantation of a Myoring
• NEW: Implantation of a Xenia® implant
Experts for this Treatment Method

- Modern Ophthalmology
Dr. Mirka R. Höltzermann
Augenpraxis Dr. Höltzermann, Dr. von Schnakenburg, Augenpraxis Dres. Höltzermann & von Schnakenburg
- Modern Ophthalmology
Dr. med. Ilya Kotomin
Smile Eyes Leipzig
- Modern Ophthalmology
Priv.-Doz. Dr. med. Daniel Pilger
Smile Eyes Berlin
- Modern Ophthalmology
Prof. Dr. med. Tanja M. Radsilber
Augenzentrum Prof. Dr. med. Holzer & Prof. Dr. med. Rabsilber
- Modern Ophthalmology
Dr. med. Karsten Klabe
Breyer, Kaymak & Klabe Augenchirurgie
- Modern Ophthalmology
Prof. Dr. med. Hakan Kaymak
Breyer, Kaymak & Klabe AugenchirurgieAll Experts in this Department
Show All
- Modern Ophthalmology
Dr. Mirka R. Höltzermann
Augenpraxis Dr. Höltzermann, Dr. von Schnakenburg, Augenpraxis Dres. Höltzermann & von Schnakenburg
- Modern Ophthalmology
Dr. med. Ilya Kotomin
Smile Eyes Leipzig
- Modern Ophthalmology
Priv.-Doz. Dr. med. Daniel Pilger
Smile Eyes Berlin
- Modern Ophthalmology
Raphael Neuhann (FEBO)
Opthalmologikum Dr. Neuhann / Augentagesklinik am Marienplatz
- Modern Ophthalmology
Dr. med. Tabitha Neuhann
Opthalmologikum Dr. Neuhann / Augentagesklinik am Marienplatz
- Modern Ophthalmology