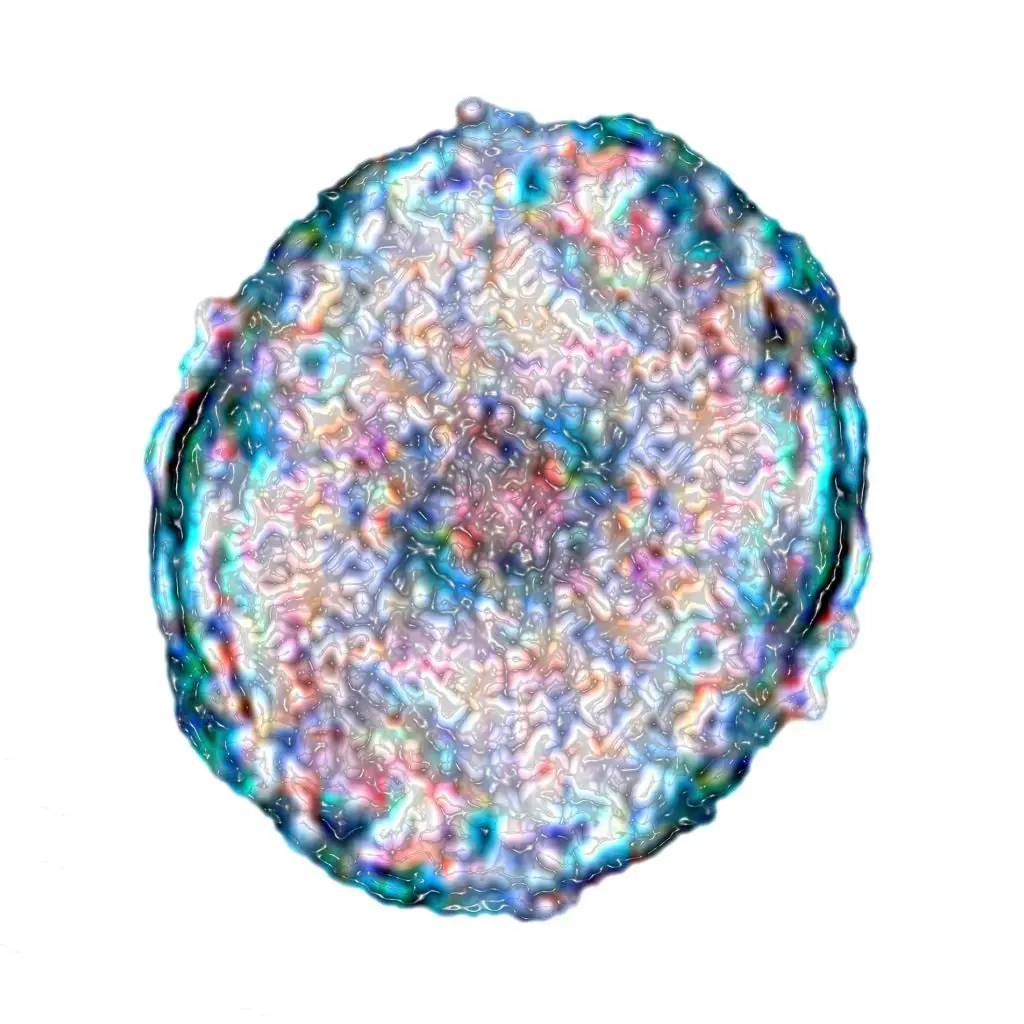
© © BSIP/ F1online
January 20, 2026
Judith Cyriax
- Health
Stem cell therapy: Which diseases can be treated with it?
From Aesthetic Medicine to Ophthalmology: How stem cells are used in therapy to replace diseased cells and regenerate tissue
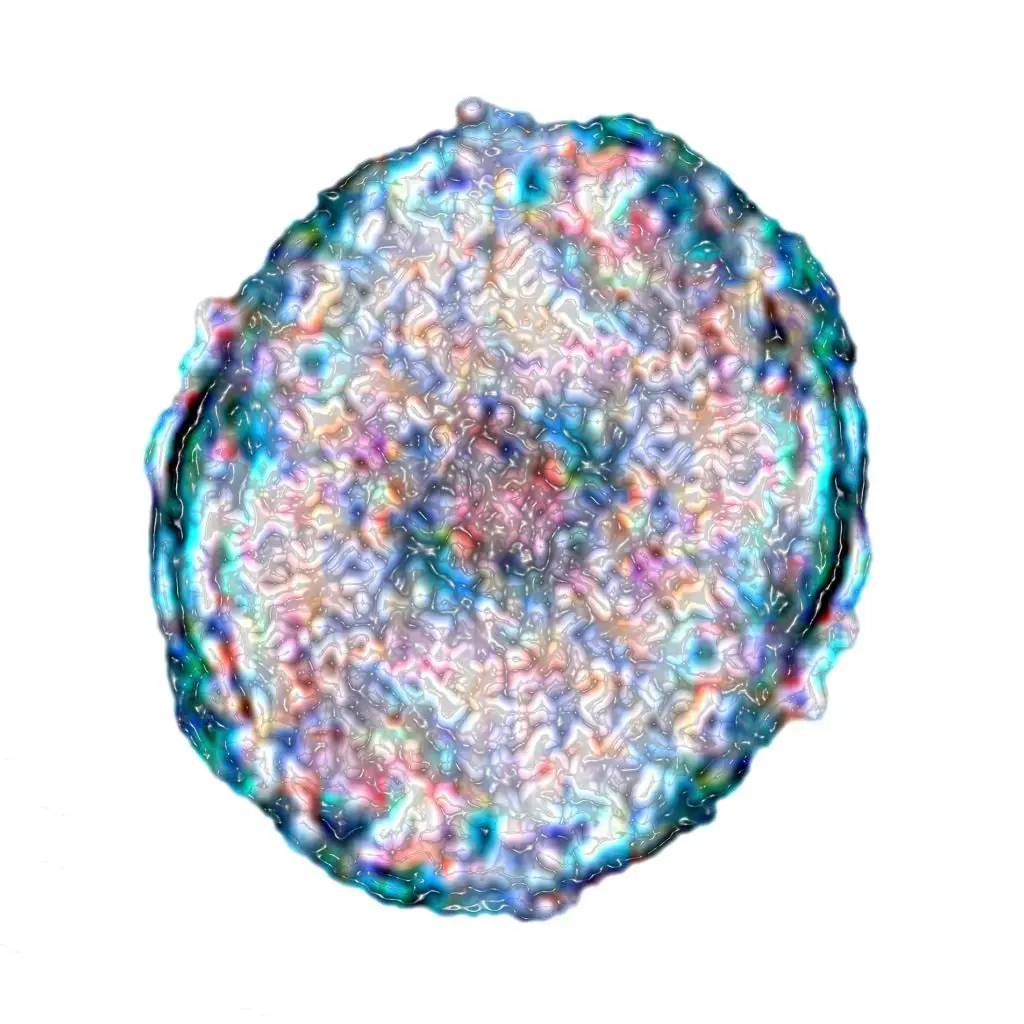
© © BSIP/ F1online
January 20, 2026
Judith Cyriax
From Aesthetic Medicine to Ophthalmology: How stem cells are used in therapy to replace diseased cells and regenerate tissue
The beginning of every life starts with a single cell – the stem cell. Tiny, yet connected with massive hopes and tremendous reservations like hardly any other topic in medical research. Both positions lie in the potential of the biological raw material: on the one hand, the prospect of having a universal building material for damaged cells, tissues, or even entire organs and being able to cure diseases such as cancer, Parkinson's, multiple sclerosis, or diabetes.
On the other hand, there is the fear that embryos – even in the very early developmental stage of a few cells – will become commodities, bred (and killed) more or less industrially for uncertain medical progress. But also that it will open the doors to cloning humans and animals – something that has been commercially successful in South Korea for years by the company "Sooam Biotech" with beloved lapdogs.
While in Germany, trade and research with embryonic stem cells have been practically completely banned by law since 2002, there are fewer or no restrictions in Asia, the USA, or even in Great Britain. Although every human has stem cells, there are significant differences in their abilities – embryonic ones are, so to speak, the all-rounders, the younger, the more talented.
In principle, stem cells are universal cells that have not yet specialized, meaning they can become all cell types in the human body: muscle, nerve, organ, and blood cells. To ensure these cell types are constantly available, the stem cell can continuously divide to create a copy of itself. However, division does not necessarily always produce two new stem cells; two different cells can also arise.
In this so-called asymmetric cell division, one of the newly formed cells is a duplicate of the mother cell and has the same properties. The other cell, in turn, develops into a specialized cell type. Unlike stem cells, these normal tissue cells cannot divide but are fixed to their assigned functions. The stem cell, on the other hand, can replace injured or diseased cells through its continuous division and thus assumes necessary regeneration and repair mechanisms in the body.
But not every stem cell is the same. Depending on their development, they are distinguished as omnipotent or multipotent. An omnipotent cell develops into a complete human, while multipotent stem cells develop into a specific tissue. Furthermore, a distinction is made between embryonic and adult stem cells. Embryonic (omnipotent) stem cells are particularly rich in so-called blood stem cells, which have the ability to develop into different types of blood cells: into red and white blood cells as well as into platelets.
For more than 30 years, it has been possible to obtain such cells from the umbilical cord blood of newborns, for example, to use them successfully in the therapy against leukemia. Around 700,000 cord blood transplants are now stored worldwide in public medical banks. Cord blood, which remains in the umbilical cord after delivery, is considered a relatively new and versatile source of various stem cells.
Contrary to popular belief, the cells in umbilical cords are not considered embryonic but are already adult stem cells. These cells are slightly influenced but are considered unburdened and divide much more frequently than adult stem cells from adults. In addition, they are much more adaptable and less likely to cause rejection reactions or infections after a transplant.
Adult (multipotent) stem cells can only form certain cell types of the human body, such as bone marrow, skin, or adipose tissue. But how could it be otherwise in the human body: The older we get, the shorter the lifespan of these stem cells and the fewer are formed. However, there are now effective methods to extract and duplicate adult cells so that they can be used in various medical fields.
Particularly great hope lies in so-called iPS cells (induced pluripotent stem cells), which are reprogrammed back into the embryonic state and thus become the original all-rounders again.
When it comes to which material is best suited for successful treatments in plastic-aesthetic surgery, stem cells are now considered the ideal solution. Whether in facial treatments (wrinkles, volume loss or sun damage), hair loss, or breast augmentation with autologous fat – the body's own raw material is proving to be increasingly effective and is being used more and more frequently. The procedure for all these interventions is similar: First, the doctor removes a small amount of autologous fat from the abdomen, thighs, or hips. This is then processed in the laboratory, meaning adult stem cells are extracted from the fat using special enzymes.
“From 100 milliliters of autologous fat, 1 million stem cells can be obtained. When these are reintroduced into the body's tissue through fine injections, they immediately begin their regenerative, reparative, and constructive work,” explains Dr. Caroline Kim, a specialist in Plastic and Aesthetic Surgery in Munich. Another advantage: “The body contains enough adult stem cells, so there is sufficient material for any intervention. Moreover, the patient does not have to fear complications, incompatibilities, or allergies, as it is autologous material,” says the expert.
In orthopedics, adult stem cell therapy is used, for example, in the treatment of osteoarthritis in the knee and hip joint. First, about 30 milliliters of fat tissue is suctioned out from the subcutaneous fat tissue using a minimally invasive procedure, and from this, the so-called mesenchymal stem cells (MSC) are extracted. These connective tissue stem cells are then injected into the joint and periarticular fat pads and can effectively resume their protective and cushioning function from there. Additionally, the tissue is renewed and inflammation is inhibited. Ideally, this therapy leads to complete pain relief and increased mobility; the use of a prosthesis can also be avoided in the long term.
Stem cells from the bone marrow (BMC) are used in cases of herniated discs. A study by the Cedars-Sinai Medical Center (Los Angeles, USA) from 2012 confirms that the injection of bone marrow stem cells improves the function of the discs, restores mobility, and reduces pain. Nevertheless, many orthopedic surgeons are still somewhat skeptical about the use of stem cells in their field. On the one hand, only mild symptoms can be treated so far, and on the other hand, the typical risks of an intervention in a joint (for example, germs from an injection) are involved.
In ophthalmology, in the near future, corneal tissue created from cultivated stem cells could restore people's vision. This is made possible by so-called iPS cells. These special cells are created in the laboratory when researchers reprogram normal tissue cells by adding genetic factors. As a result, they have similar properties to embryonic stem cells and can develop into any cell in the human body.
For this discovery, the Japanese Shinya Yamanaka received the Nobel Prize for Medicine in 2012, and already in 2014, Japanese ophthalmologists implanted retinal cells into the eye of a woman who suffered from an age-related form of blindness, which were cultivated from iPS cells. The transplantation halted the progression of the disease and had hardly any side effects.
And this is exactly where the hope of ophthalmology in relation to stem cell therapy lies: the development of a cornea. Corneal transplantation (keratoplasty) remains the most frequently performed transplantation. According to the German Ophthalmological Society (DOG), more than 9,000 corneas are transplanted each year, with each cornea helping two people regain their vision. However, there are too few donors, so cultivated corneas would be the perfect way to help more people.
Stem cells are among the most promising research fields in modern medicine. Their unique ability to develop into different cell types and regenerate damaged tissue opens up therapeutic possibilities that were unthinkable just a few decades ago. From the treatment of osteoarthritis to aesthetic applications to the restoration of vision—the practical applications are steadily growing.
The development of iPS cells (induced pluripotent stem cells) in particular represents a scientific breakthrough that largely bypasses ethical concerns associated with embryonic stem cells. These reprogrammed adult cells combine the versatility of embryonic stem cells with the ethical soundness of body-derived material. The fact that this discovery was awarded the Nobel Prize in 2012 underscores its significance for the future of medicine.
Despite all progress, stem cell therapy is still in the developmental phase in many areas. Long-term studies are partly lacking, success rates vary, and not all medical fields are equally convinced of its effectiveness. Moreover, the legal situation remains inconsistent internationally—while Germany pursues strict regulations on embryonic stem cells, other countries take a more liberal approach to research.
The coming years will show to what extent stem cells can realize their potential in practice. For patients with previously incurable diseases, they mean one thing: hope for healing or at least significant improvement in their quality of life. The path from research to standardized therapy may still be long, but the direction is promising.