Diabetes is considered a widespread disease. Around 11 million people in Germany suffer from it. How to live with this metabolic disorder with as few restrictions as possible and whether the disease will be curable in the future, I discuss with Dr. Alexandra Schoeneich, specialist in endocrinology, diabetology, and internal medicine at the Diabetes, Hormone, and Metabolism Center at Isar Klinikum Munich.
Diabetes as a widespread disease: What does that mean?
Diabetes is referred to as a widespread disease. What exactly is meant by that?
Dr. Schöneich: The fact that diabetes is one of the most common chronic diseases in Germany and the incidence is unfortunately still increasing.
There are types 1, 2, and 3 diabetes, as well as pregnancy and gestational diabetes. Are the symptoms the same for all?
Dr. Schöneich: Yes. It leads to increased blood sugar.
Types 1, 2, and 3 diabetes: The differences explained
Can you briefly explain how the types differ and what percentage of people are affected?
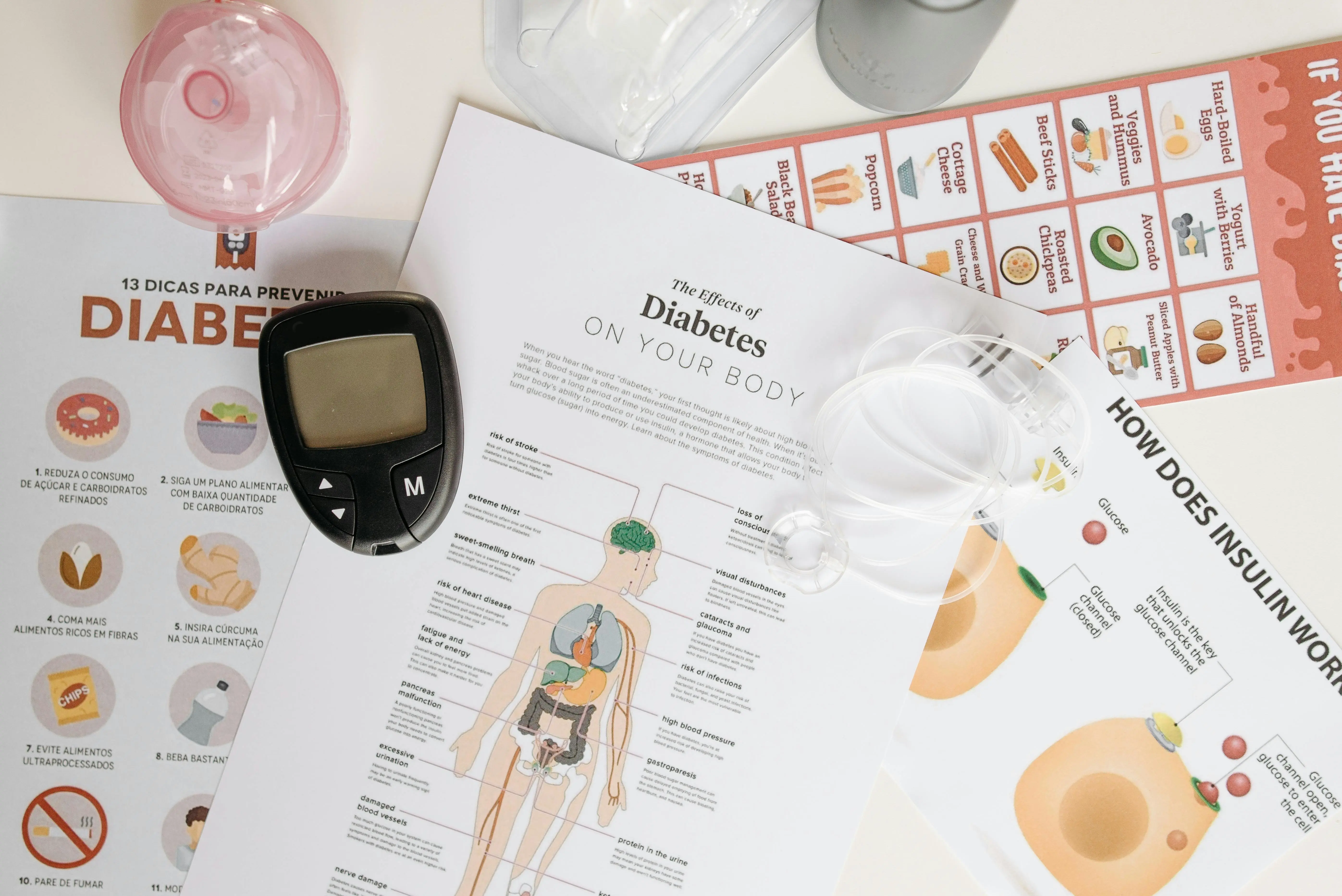
Dr. Schöneich: Type 2 diabetes is the most common of all types of diabetes, occurring in 95% of cases. It is a type of diabetes that develops insidiously over many years. Therefore, prevention is crucial and very, very important here. Ultimately, type 2 diabetes develops through insulin resistance. Insulin is actually responsible for keeping blood sugar stable in the blood.
When insulin no longer works as well, less sugar is absorbed into the cells. This leads to an increase in blood sugar, which we call insulin resistance. If insulin resistance persists for many years, an additional insulin deficiency develops.
The pancreas becomes weaker and produces less insulin, thus releasing less as well. Blood sugar continues to rise. Type 2 diabetes is also promoted by lack of exercise, weight gain, or being overweight. That's why prevention is so crucial here.
And what about Type 3?
Dr. Schöneich: First, I'll briefly return to Type 1 diabetes, a rare form of diabetes. It is an autoimmune disease and affects only about 5% of diabetes cases. Type 1 diabetes primarily occurs in childhood and young adulthood, but it can occur at any age.
The autoimmune disease results in the formation of antibodies in the body that lead to the destruction of beta cells, the insulin-producing cells in the pancreas. This then leads to an insulin deficiency. This type of diabetes always requires insulin therapy.