Other Treatment Methods
- 4D static analysis and dynamic pedography
- Acupuncture
- Arthrosis therapy
- Artificial elbow joint
- Artificial hip joint
- Artificial knee joint
- Artificial shoulder joint
- Axomera
- Bioregenerative Orthopedics
- Endoprosthetics
- IHHT and stress analysis
- Medical training therapy
- Open MRI and MRI-guided injection therapy
- Orthopedic pain therapy
- Osteopathy
- Shock wave therapy
- Sports orthopedics / sports medical treatment

Artificial knee joint
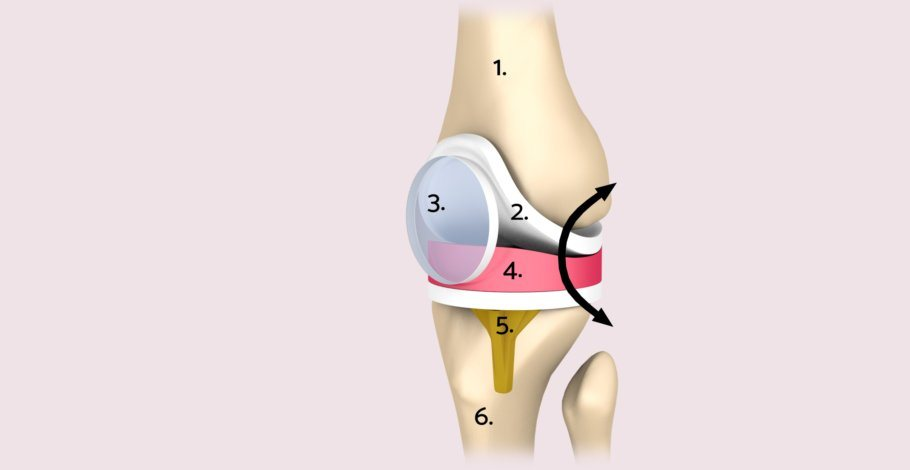
The human knee joint is a highly complex mechanical structure. Four bones come together here: the femur, tibia, fibula, and the patella. Together they form – functionally speaking – three joints: the medial and lateral joints between the thigh and lower leg, as well as the joint between the femur and patella. All sub-joints can theoretically be replaced individually with artificial joints.
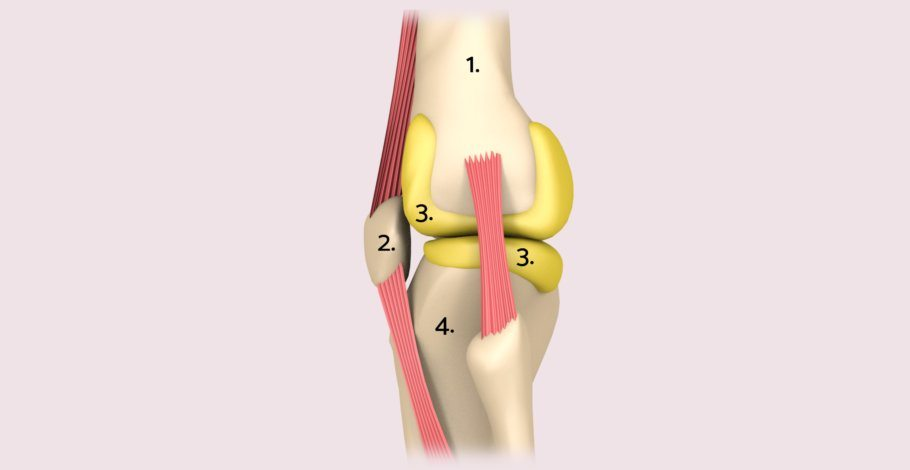
The knee joint can bend and stretch like a hinge, but also allows rotational movements when bent. Lateral, medial, and cruciate ligaments, as well as the strong musculature provide the knee joint with its stability despite long lever ratios. A bony guidance, as for example with the hip joint, is not present.
Osteoarthritis as a reason for an artificial knee joint
About 150,000 people in Germany decided in 2015 for an artificial knee. The procedure should be well thought-out, but not postponed for too long. The further the osteoarthritis progresses, the more technically challenging it is to fit a new joint. Additionally, functional abilities such as strength, flexibility, and gait symmetry are lost during the disease process, complicating both the operative procedure and postoperative care.
Which prosthesis as an artificial knee joint?
Depending on the functional condition of the affected joint (especially the ligaments), Age and the patient's health status, as well as other factors, doctors can offer their patients different prosthetic models. The options range from partial replacement to axis-stable total prosthesis:
• Unilateral (unicondylar) surface replacement, also known as a sled prosthesis
• Complete (bicondylar) surface replacement, also referred to as knee joint total endoprosthesis or knee-TEP
• Complete knee joint replacement with an axis-guided, stemmed prosthesis
The total endoprosthesis of the knee joint (knee-TEP)
In Germany, doctors implant approximately 150,000 total endoprostheses (TEP) in their patients annually. This makes the knee, after the hip TEP, the second most common prosthesis in which the joint is completely replaced. The most commonly used models, which also deliver the best functional results, require the patient’s intact, functional ligament apparatus. In an ideal situation, the surgical procedure takes about 45 to 60 minutes.
Partial prosthesis (sled) of the knee joint
Experts speak of a sled or partial prosthesis when only half of the knee joint is replaced. The attending physician chooses this joint replacement if, for example, due to malalignment (bow-leg or knock-knee), the joint is arthritically altered on only one inside or outside. Usually, the inside part is affected. The remaining parts of the knee joint must still be in very good condition for this type of prosthesis. A sled prosthesis is also only an option if the stabilizing ligament apparatus is completely intact and functional.
Axis-guided knee joint endoprosthesis
For some patients, the previously mentioned prostheses are not an option because the knee would not be stable enough after this type of replacement. There are the following reasons for this:
• The bone is already very weakened due to diseases such as bone loss (osteoporosis).
• The leg axis deviates massively from its ideal position due to leg misalignments (bow-legs, knock-knees).
• The lateral and cruciate ligaments are unstable, for example, after a previous accident or during a revision surgery.
In these cases, the surgeon has a so-called axis-guided (coupled) knee joint endoprosthesis available. Here, the implant takes over the task of the ligaments: The upper and lower leg parts of the prosthesis are connected by an axis and each provided with a long shaft that the doctor can safely anchor in the bone.
Axis-guided knee joint endoprostheses always represent a compromise: They offer stability and secure anchorage but have functional disadvantages because the mobility of the knee is thus restricted.
Knee prosthesis with or without patellar surface replacement
Even the important joint between the kneecap and thigh bone can cause severe pain when worn out, for example when descending stairs, directly behind the kneecap. During a knee joint endoprosthesis operation
the condition of the joint surfaces there is always checked. Depending on the findings, the surgeon can decide:
• He removes the arthrotically altered joint surface on the back of the kneecap and replaces it with a polyethylene plastic implant.
• He performs a so-called joint lavage and removes bone spurs and ridges as well as any other disruptive tissue.
• He does not need to take any surgical measures on the back of the kneecap.
Artificial knee joint tailored to measure
In addition to completely prefabricated prosthesis models in different sizes, some manufacturers have been offering individually shaped prostheses for a few years. The term encompasses various variants. On the one hand, there are special prostheses for Women, which are intended to meet the geometric requirements of the female knee joint.
In addition, surgeons can access customized prostheses tailored exactly to the anatomical specifications of the individual patient. This "custom-made endoprosthesis" is produced in several steps: First, a radiologist performs a special computed tomography (CT) from the hip to the foot to precisely capture the anatomical structure of the knee joint and the leg axes. Based on the determined data, a 3D model of the knee joint replacement is created using software, which considers the joint's individual shape as well as the arthritis distribution pattern. The data is sent by the doctor to the manufacturer, who produces the individual templates and tools as well as the prosthesis within 4 to 8 weeks. Although it is believed that the custom knee joint endoprosthesisEndoprothese lasts longer and functions better due to its improved fit, this has not yet been confirmed by sufficient data.
Best materials for knee prostheses
To ensure long-lasting durability and good compatibility, endoprostheses must meet various requirements: They must be able to anchor ideally in the bone. The foreign substances used should not cause any adverse reactions and must be corrosion-resistant. The sliding of the artificial joint surfaces should lead to as little abrasion as possible, as this can damage the surrounding tissue. Metals (titanium, stainless steel alloys), plastics (polyethylene), and ceramics are used in the production of endoprostheses.
Procedure of the Knee Joint TEP Operation
The endoprosthetic replacement of the knee joint takes place under general anesthesia or in what is known as spinal anesthesia, where pain and sensation in the surgical area are eliminated but the patient remains conscious. The decision is made by the anesthesiologist in a pre-operative discussion with the patient. After positioning and disinfecting the area, the joint is exposed through a longitudinal incision over the front of the knee. As the surgeon progresses towards the joint, muscles, tendons, and ligaments are protected.
The defective joint surfaces are removed, and the bone is prepared so the artificial joint components can be stably anchored. The surgeon uses special templates to help him remove the right amount of bone for the implant. The prosthesis model specified in the surgical plan is then inserted and checked for functionality, with stability and mobility being crucial for the patient's later satisfaction in everyday life and the longevity of the artificial joint. The new components are either precisely pressed into the prepared surface or anchored with so-called bone cement (acrylic resin, polymethylmethacrylate).
Minimally Invasive Knee Joint TEP?
The term "minimally invasive surgery" ("keyhole surgery") is known from abdominal or spinal surgery and other areas of application. The desire of patients for the smallest possible, cosmetically attractive scars is great. In knee joint surgery, arthroscopic procedures have also become established, for example, for meniscus and cruciate ligament operations, but not in endoprosthetics. This is because smaller skin incisions offer the surgeon less visibility, poorer orientation, and more difficult hemostasis. Therefore, each surgeon decides for themselves how small or large to make the skin incision.
Knee joint TEP with or without navigation?
Navigation systems for endoprosthetic surgery have been available since around 2000. Using infrared cameras, the surgeon receives exact information on the individual conditions of the patient, such as the optimal positioning of the cutting planes, the three-dimensional orientation of the prosthetic components, and the depth of bone resection. Navigation systems are more accurate, with deviations of 0.5° or 0.5 mm than the human eye or conventional instruments. However, they also have their disadvantages: the operation takes longer, and the technical effort is greater.
After the surgery
On the first day after the operation, the operated knee joint is carefully moved by a physiotherapist or with the help of a motorized rail. At the same time, gait training begins with forearm crutches or a walker.
The hospital stay averages about seven days, longer in the event of complications or after a revision surgery. This is followed by several weeks of rehabilitation.
Experts for this Treatment Method

- Innovative Orthopedics & Sports Orthopedics
Dr. med. Martin Volz & Kollegen
Sportklinik Ravensburg
- Innovative Orthopedics & Sports Orthopedics
Prof. Dr. med. Dieter Christian Wirtz
Klinik und Poliklinik für Orthopädie und Unfallchirurgie
- Innovative Orthopedics & Sports Orthopedics
Prof. Dr. med. Henning Windhagen
DIAKOVERE Annastift
- Innovative Orthopedics & Sports Orthopedics
Univ.-Prof. Dr. med. Rüdiger von Eisenhart-Rothe
Klinik für Orthopädie und Sportorthopädie, Klinikum rechts der Isar
- Innovative Orthopedics & Sports Orthopedics
Prof. Dr. Hans-Georg Simank
Zentrum für Orthopädie und Neurochirurgie
- Innovative Orthopedics & Sports Orthopedics
Prof. Dr. med. Sebastian Siebenlist
Sektion Sportorthopädie TU München, Klinikum rechts der IsarAll Experts in this Department
Show All
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Florian Pfalzer
Sportpraxis Stuttgart / Health & Aesthetic Stuttgart
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Ivo Breitenbacher
MVZ für Orthopädie Flugfeld
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Yvonne Ebel
Orthopädie Wernau
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Konrad Scheuerer, Dr. med. Ulrich Bader
OrthoPraxis Gräfelfing
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Martin Volz & Kollegen
Sportklinik Ravensburg
- Innovative Orthopedics & Sports Orthopedics