Other Treatment Methods
- 4D static analysis and dynamic pedography
- Acupuncture
- Arthrosis therapy
- Artificial elbow joint
- Artificial hip joint
- Artificial knee joint
- Artificial shoulder joint
- Axomera
- Bioregenerative Orthopedics
- Endoprosthetics
- IHHT and stress analysis
- Medical training therapy
- Open MRI and MRI-guided injection therapy
- Orthopedic pain therapy
- Osteopathy
- Shock wave therapy
- Sports orthopedics / sports medical treatment

Artificial hip joint
The hip joint is a special form of a ball joint and, as such, allows movement in all planes of space. Due to its central location near the middle of the body, it plays an important role in all activities of life. Activities of life – Pain and movement restrictions of the hip joint therefore particularly affect us. They are often the result of hip joint osteoarthritis or coxarthrosis, in which the joint wears out over a longer period of time.
Arthritis as a reason for an artificial hip joint
Normally, a complete, elastic, perfectly smooth cartilage layer covers the joint head and socket. Cartilage enables smooth movements and absorbs shocks. It is mainly nourished by the joint fluid since it has no blood vessels of its own. The wear process in arthritis is mainly triggered by overweight, lack of exercise, repeated overloads, and accidents. Patients usually notice this through gradually increasing pain during or after physical activities such as long walks, descending hills, or climbing stairs. Upon closer examination, movement restrictions in the hip joint can often be detected. They begin largely unnoticed but characterize the picture of advanced hip osteoarthritis.
Artificial hip joint after femoral neck fracture
Three-quarters of artificial hips become necessary because arthritis, the wear process, has severely damaged the joint. Another 50,000 artificial hips are used by trauma surgeons and orthopedists after patients have suffered a femoral neck fracture. Most patients who decide on an artificial hip have over the age of 70. About one-fifth of patients with a new hip joint, however, are younger than 50 years.
Which prosthesis as an artificial hip joint?
The hip joint endoprosthesis is one of the most common and successful surgical procedures in medicine in general: About nine out of ten operated patients are happy after joint replacement about a pain-free life with normal mobility. In the 1960s, with the development of artificial hip joints, their routine installation began. Other joints such as knee, shoulder and ankle joint followed. A decisive step was the introduction of "bone cement" (actually acrylic resin, polymethyl methacrylate) in 1964 to anchor the foreign material in the bone.
What is the artificial hip joint made of?
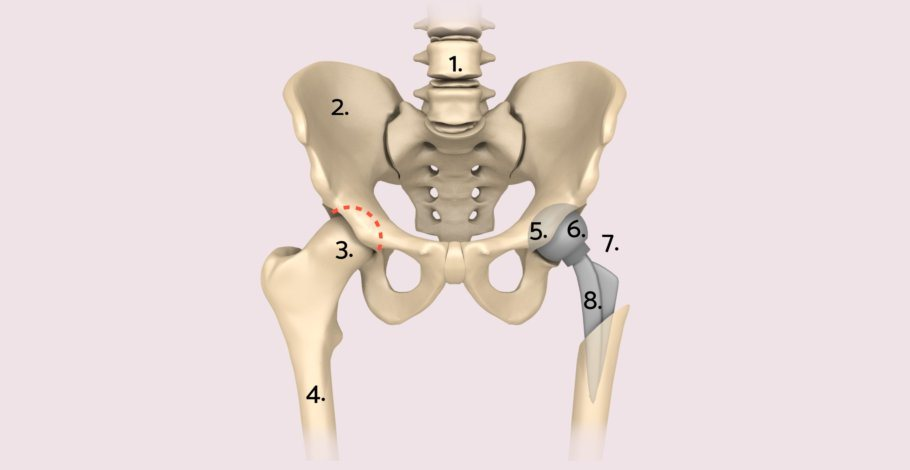
Today, doctors and patients can choose between different models, materials, as well as surgical options and anchoring techniques. Most often, the artificial joint consists of a stem-shaped shaft that is attached to the femur. A head is placed on the neck of the shaft. The counterpart forms the artificial socket. Different materials are available for all components. Shaft and socket can be anchored with or without cement – or both methods are combined in the so-called hybrid endoprosthesis.
Today, with one exception, only total prostheses are used. Other methods have not proven themselves. The aforementioned exception is the so-called duo-head prosthesis, which consists of shaft, head, and socket in one unit and is only anchored in the shaft. The artificial socket slides in the unchanged hip socket of the patient. This model is mainly used for femoral head replacement after femoral neck fracture. Its advantage is the shorter operation time.
Total endoprosthesis of the hip joint (Hip-TEP)
The typical, by far most frequently used total hip joint endoprosthesis (short: Hip-TEP) consists of three components: the femoral shaft, the hip socket, and the joint head that sits on the femoral shaft. In the procedure, the arthritically changed joint parts are removed and replaced with implants. The surgical intervention ideally lasts between 40 and 50 minutes.
The hip sockets used for a hip joint endoprosthesis today mostly consist of a metallic shell, usually made of titanium, and the inlay made of highly cross-linked polyethylene (alternatively ceramic). The surgeon presses the shell into the bone either cement-free (so-called press-fit method) or anchors it with bone cement. In difficult conditions, he can additionally anchor the shell with screws. Special socket models are available to him for this purpose.
The prosthesis shaft consists of stem, body, and neck. The stem varies in length depending on the model; different shape variants are also available. The body and stem of the prosthesis shaft are anchored in the medullary cavity of the femur. Here too, there is the option to do this cement-free or with the help of bone cement. The ceramic head is placed on the conically shaped prosthesis neck. In many cases, immediate full weight-bearing after prosthesis insertion is possible. In difficult conditions, it may be necessary to relieve (partially load) the operated leg with forearm crutches for a few weeks.
Cement-free short-stem prostheses for the Hip-TEP
For several years, surgeons have also been using cementless short-shaft prostheses. As the name suggests, the stem of the short shaft is shorter than that of conventional prostheses. Short shafts usually follow a different biomechanical principle than long shafts. The idea behind this is that if an implant is later required to be replaced, more bone is available to the surgeon to securely anchor the subsequent implant. The removal of the prosthesis might also be easier. Since such a replacement is more likely in younger people, short shafts are particularly used in them.
Materials in total hip arthroplasty (THA)
Metals (titanium, stainless steel alloys), plastics (polyethylene), and ceramics are used in the manufacture of endoprostheses. The main requirements for an implant during its stay in the body are biocompatibility and biofunctionality. The durability of the hip prosthesis is primarily determined by the combination of materials that slide directly against each other during movement (so-called sliding pairs). The most common combination used is the ceramic-plastic sliding pair: the harder prosthesis head made of ceramic slides in the softer insert made of highly cross-linked polyethylene.
Surface replacement in artificial hip joint (cap prosthesis, McMinn prosthesis)
In rare exceptional cases, instead of implanting a femoral shaft, only the damaged hip joint head is crowned. As a result, the prosthesis head placed on the femoral neck is relatively large. To keep the loss of substance in the pelvis low, a very thin metal cup is used. This creates a sliding pair of metal (hip head) and metal (joint cup).
The advantages of this concept lie in less loss of bony substance, absence of plastic wear, and low risk of dislocation. The disadvantage is metal wear, which can lead to local (granulomas) or systemic (allergy, heavy metal poisoning) foreign body reactions. Currently, this method is a rarely chosen alternative to the classic total hip arthroplasty (THA).
Dual head prosthesis (after femoral neck fracture)
A femoral neck fracture is usually treated surgically today. The surgeon has several methods at their disposal to achieve a stable connection of the broken bone parts. If the patient's joint cannot be preserved, an endoprosthetic joint replacement is an option. Depending on the degree of damage, either only the hip head (dual head prosthesis) is replaced or both the hip head and cup (total endoprosthesis, see there). The dual head prosthesis offers advantages, especially in the treatment of older people:
• shorter operation times, shorter anesthesia duration
• Lower blood loss.
• Lower surgical risk / lower complication rate.
The stem of the dual-head prosthesis can be cemented or cementless anchored.
Procedure of the operation for hip TEP.
In hip endoprosthetics, three main approaches are used: anterior, lateral, and posterior access. There are pro and con arguments for all accesses. The surgeon decides which access route he considers the most suitable. He removes the diseased joint parts and instead inserts artificial elements. These are usually the hip socket and hip shaft. The hip socket is inserted into the pelvis and fixed there (cemented, pressed, or screwed). The hip shaft is given a ball head.
Minimally invasive hip TEP?
In recent years, soft tissue-saving, minimally invasive access routes have become established worldwide in operative medicine. The aim of using these techniques is for patients to have smaller scars, less pain, and less blood loss.
Endoprosthetic surgery places various demands on the surgeon. In addition to exposing the operating area as gently as possible on the tissue, careful blood stasis, axis-appropriate positioning of the cutting planes, the implants must be placed three-dimensionally correctly. For this, a sufficient field of view of the operating field is required. In this respect, minimal invasive techniques have limits set. Unlike in the rest of surgery, the term minimally invasive endoprosthetics does not refer solely to the length of the skin incision, but also to maximum skimping on the muscles and other tissue structures of the hip joint.
The further development of instruments and diverse experiences with minimally invasive techniques has now led to the fact that, in most cases, operations can be performed with significantly shorter skin incisions, without neglecting criteria of care.
Total hip endoprosthesis with navigation
In everyday clinical practice, so-called imageless navigation systems have become established. They use infrared cameras and do without burdensome X-ray radiation. They provide orthopedic surgeons with the opportunity to reliably control the three-dimensional position of the individual components. The goal of using navigation systems is implant positioning that is aligned with the patient's individual anatomy and thus leads to improved postoperative function and optimized range of motion.
Risks of total hip replacement
The renowned medical journal Lancet called joint replacement the "operation of the 21st century" in 2007. Prostheses now last an average of 15 to 20 years, often longer. Aside from the durability of the prosthesis, potential complications are of interest for the success of an artificial joint. Some of the most serious risks of joint replacement surgery include:
• Infections (early, late; superficial, deep),
• The formation of blood clots in a leg vein (thrombosis, possibly embolism)
• So-called aseptic prosthetic loosening (without infection)
Risk of infections and thromboses after a hip TEP
Critical for the prognosis is the earliest possible detection of a complication and its immediate, appropriate treatment. Infections require treatment with antibiotics. With deep infections, partial or complete removal of the prosthesis may be necessary. Thromboses are detected with special ultrasound examinations and treated with medications that reduce the blood's clotting ability.
Annually, approximately 24,000 artificial hips and around 16,000 artificial knees are replaced in Germany. In about half of the cases, an infection is the underlying cause, and additionally, aseptic loosening (loosening without infection) and other mechanical causes are responsible for the prosthesis exchange.
The German Society for Orthopaedics and Orthopaedic Surgery (DGOOC) has certified operation centers that ensure experienced surgeons oversee all procedures, all steps are documented, and the staff is regularly trained. The case numbers of the centers are publicly accessible.
After the operation
Early rehabilitation begins in the hospital immediately after the procedure: Gait training with forearm crutches or a walker under physiotherapeutic guidance starts the day after the operation. In some cases, the surgeon prescribes (partial) relief of the operated leg for a few weeks. The hospital stay is on average about seven days, but longer in case of complications or after a prosthesis exchange operation. Following the hospital stay, a multi-week rehabilitation is necessary to enable a quick and successful return to everyday life.
Movement without pain after hip TEP
After an artificial joint replacement, pain-free movement should ideally be possible without walking aids within six to eight weeks, but no later than three months. Moderate sporting activities (hiking, walking, golf, cycling, swimming, strength training, etc.) are usually no problem. However, artificial joints are not sports joints and should be treated with care and caution. The better this is achieved, the higher the chances that an artificial joint will last for many years, ideally a lifetime.
The behavior and lifestyle of the patient are also crucial for the success of the treatment. Weight control, strength building, coordination training (gait image), as well as the type and extent of daily use are factors that are solely in the hands of the patient.
Rehabilitation measures after total hip arthroplasty
A multi-week intensive rehabilitation begins immediately after the hospital stay (usually one week after the operation). It is intended to ensure a continuous healing process and a goal-oriented development of the patient's motor skills. Here, pain is treated, wound healing is monitored, the muscles are stabilized, and coordination is trained. Health status, home care, and possible complications determine whether a patient undergoes rehabilitation in an inpatient (stay at the rehabilitation clinic with full care and therapeutic applications) or outpatient form (living at home, treatments at one or more therapeutic facilities). The organization of rehabilitation is handled by the hospital's social service in coordination with the surgeon and patient; the cost is covered by health insurance.
Experts for this Treatment Method

- Innovative Orthopedics & Sports Orthopedics
Dr. med. Konrad Scheuerer, Dr. med. Ulrich Bader
OrthoPraxis Gräfelfing
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Martin Volz & Kollegen
Sportklinik Ravensburg
- Innovative Orthopedics & Sports Orthopedics
Prof. Dr. med. Dieter Christian Wirtz
Klinik und Poliklinik für Orthopädie und Unfallchirurgie
- Innovative Orthopedics & Sports Orthopedics
Prof. Dr. med. Henning Windhagen
DIAKOVERE Annastift
- Innovative Orthopedics & Sports Orthopedics
Univ.-Prof. Dr. med. Rüdiger von Eisenhart-Rothe
Klinik für Orthopädie und Sportorthopädie, Klinikum rechts der Isar
- Innovative Orthopedics & Sports Orthopedics
Prof. Dr. Hans-Georg Simank
Zentrum für Orthopädie und NeurochirurgieAll Experts in this Department
Show All
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Florian Pfalzer
Sportpraxis Stuttgart / Health & Aesthetic Stuttgart
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Ivo Breitenbacher
MVZ für Orthopädie Flugfeld
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Yvonne Ebel
Orthopädie Wernau
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Konrad Scheuerer, Dr. med. Ulrich Bader
OrthoPraxis Gräfelfing
- Innovative Orthopedics & Sports Orthopedics
Dr. med. Martin Volz & Kollegen
Sportklinik Ravensburg
- Innovative Orthopedics & Sports Orthopedics