Gynecological check-up
The preventive medical check-up usually includes several standardized steps. First, the medical history is taken, in which the following points are clarified: the course of the menstrual cycle, Pregnancies, births, and miscarriages, Contraceptive methods, possible physical complaints. Family predispositions are inquired (keyword breast- or ovarian cancer), and one's own lifestyle is discussed.
Examination of the sexual organs including Pap test
The examination begins with the inspection of the labia, followed by the inspection of the vagina and cervix (cervical canal) using a speculum and the collection of smears for the Pap test. The Pap test, also known as a Pap smear or Papanicolaou test, is used to detect early signs of cervical cancer or its precursors. Cells are taken from the cervix and cervical canal with a spatula or a long cotton swab and then examined under a microscope in the laboratory for changes.
The Pap test is part of regular cancer screening and is offered annually in Germany from the age of 20. From the age of 35, in addition to the Pap test, an HPV (human papillomavirus) test is also performed - the main cause of cervical cancer. The examination concludes with a manual examination, where the uterus, ovaries, and fallopian tubes are palpated to identify possible changes or pain.
The ultrasound
The ultrasound examination at the gynecologist is a non-invasive method to examine the internal reproductive organs such as the uterus, ovaries, and fallopian tubes. It is performed either through the vaginal method (more frequently) or the abdominal method (over the abdominal wall). During the vaginal examination, an ultrasound probe covered with gel is carefully inserted into the vagina. The probe generates high-frequency sound waves, which display an image of the organs on the monitor. The doctor checks the form, size, and thickness of the uterine lining and examines the ovaries in terms of position, size, possible cysts, or tumors. If necessary, abnormalities like fibroids, polyps, fluid accumulations, or signs of endometriosis are investigated.
During the abdominal ultrasound, an ultrasound gel is applied to the lower abdomen to improve the transmission of sound waves. The transducer is then moved over the abdominal wall to visualize the uterus and ovaries. Abdominal ultrasound is mainly used in pregnant women, also to examine the fetus.
The breast examination
The breast examination is used for the early detection of changes such as lumps, hardening, or other abnormalities that could indicate breast cancer or other diseases. The procedure is standardized and takes place in two steps: During the visual examination, the specialist looks at the breast in different positions. First, the patient lets her arms hang loosely, lifts them above her head, and places her hands on her hips. During this, skin changes such as redness or swelling are assessed and whether the nipple shows abnormalities such as retractions or inflammations. It is also checked whether there are differences in size and shape between the breasts. During the palpation of the breast, the doctor or physician systematically palpates the breast with flat fingers, always from the outside in, to cover the entire breast. Special attention is paid to the upper outer quadrants, as breast cancer most often occurs there. In addition, the nipples are gently squeezed to check for possible secretion. The lymph nodes in the armpits and along the collarbone are also palpated, as enlarged or hardened lymph nodes could indicate diseases.
STD test and HIV test
.
An STD test (Sexually Transmitted Diseases) is used to detect sexually transmitted infections (STIs) such as chlamydia, gonorrhea, syphilis, HIV, hepatitis B and C, herpes, or HPV. The tests are conducted depending on the suspected diagnosis, symptoms, or individual preference. An STD test is always useful when symptoms like unusual discharge, burning, itching, or pain occur during urination/sexual intercourse. Testing can also be done after unprotected sex or a change of partner. As part of prenatal care, the STD test can be conducted alongside standardized tests like HIV, syphilis, or hepatitis B.
The testing procedure depends on the suspected infection and can vary. For example, to test for chlamydia or gonorrhea, cells and secretions are taken from the vagina, cervix, or urethra. A urine sample can also provide information. Blood samples are taken to detect antibodies or pathogens if HIV, syphilis, herpes, or hepatitis B/C is suspected. All samples are sent to a laboratory for examination for specific pathogens. Results are typically available within a few days.
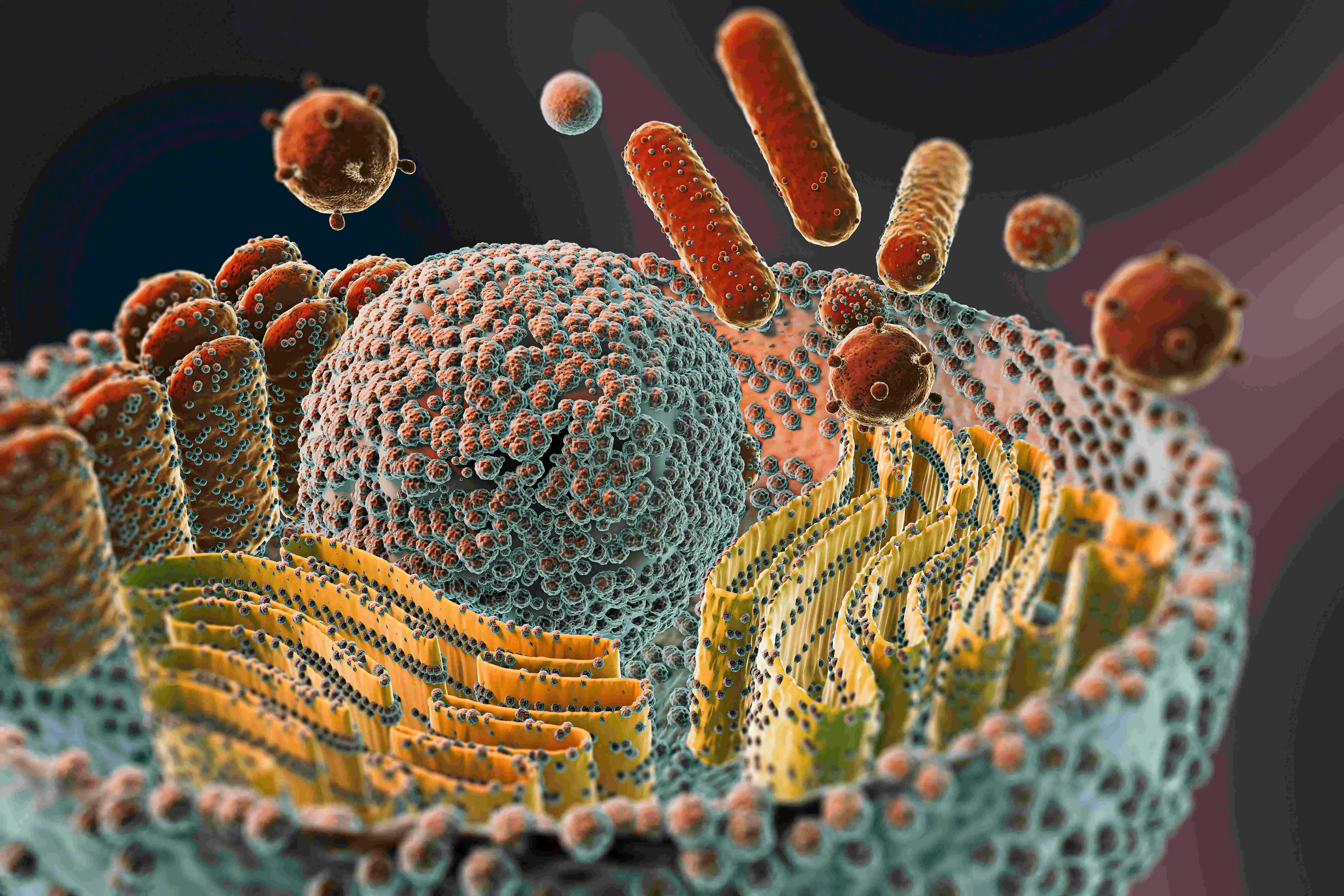
HPV vaccination
The vaccination against HPV is a protective vaccination against certain types of human papillomavirus (HPV), which are responsible for the development of cervical cancer and other HPV-related diseases. It is one of the most important preventive measures in gynecological care. HPV is a group of more than 200 virus types. Some of them are known as high-risk viruses because they cause cell changes and cancer can trigger. The virus can be transmitted through skin and mucous membrane contact, especially during sexual intercourse. The aim of the HPV vaccination is therefore to prevent infections with high-risk HPV types.
The Standing Committee on Vaccination (STIKO) in Germany recommends HPV vaccination for girls and boys between the ages of 9 and 14. The optimal time is before the first sexual contact, as full protection is only given if the infection with HPV has not yet occurred. Catch-up vaccinations are possible up to the age of 17.
Tumor markers
Tumor markers are substances that can appear at increased concentrations in the blood or other body fluids in certain cancers. In gynecological preventive examinations, tumor markers play more of a supplementary role and are not a standard service of statutory cancer screening. Why is this so? Tumor markers are not reliable enough to use routinely, as they can also be elevated in benign diseases or inflammations. However, if cancer is suspected based on symptoms or imaging findings, they can be used to support the diagnosis. Furthermore, they are used to monitor the response to therapy after cancer treatment.