Other Treatment Methods
- Dental anxiety / pain-free dental treatment
- Dental prosthesis
- Digital dentistry
- Gum treatment
- Orthodontics
- Pediatric dentist
- Prophylaxis / Professional Teeth Cleaning (PZR)
- Root canal treatment / Endodontics
- Sports dentistry
- Teeth grinding and CMD (Craniomandibular Dysfunction)
- Teeth whitening / Bleaching
- Veneers (dental shells)

Gum treatment
The doctors of Premium Medical Circle offer various types of gum treatments.
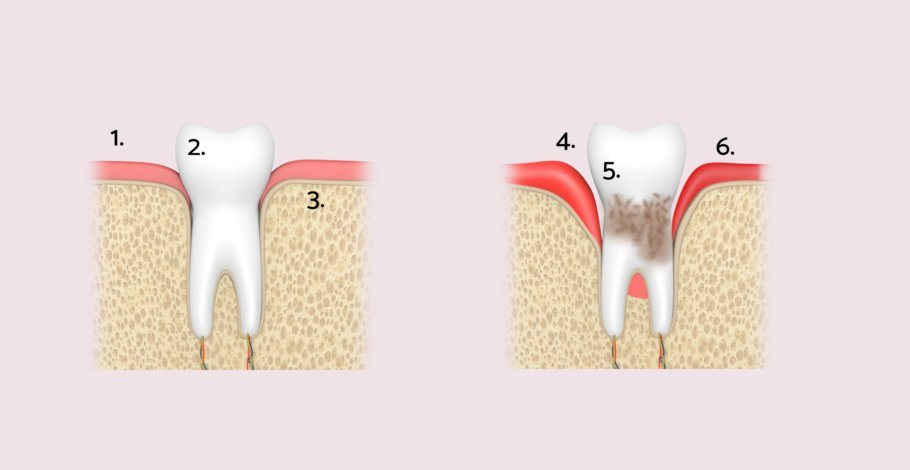
Periodontitis / periodontal disease
Periodontitis (PA) is an inflammation caused by bacteria, which, depending on the severity, can also result in irreversible destruction of the supporting structure of the tooth (periodontium). Commonly, it is referred to as periodontal disease. Gingivitis is an inflammation of the periodontium, from which periodontitis can develop. The first signs of inflammation are redness, swelling, and gum bleeding.
Symptoms of periodontitis and gingivitis
Periodontitis is triggered by bacterial plaque, like gingivitis. The main distinguishing feature of the two diseases: periodontitis involves existing, radiologically detectable bone loss; with gingivitis (gum inflammation), the deepened gum pockets are a result of inflammatory swelling of the gingiva. A long-lasting gum inflammation can extend to the jawbone, the root membrane, and the cementum. However, the transition is not mandatory. Both in gingivitis and periodontitis, metabolic and decay products are released from the biofilm, triggering the body's defense reaction.
Thus, the immune system plays the main role in tissue destruction immune system, which tries to eliminate the bacteria. This results in enzymes being formed that aim to destroy bacteria - however, they also lead to the destruction of body tissue. Ultimately, this leads to the loss of connective tissue and bone. The consequences are bleeding gums, pocket formation, receding gums, and eventually loosening or even loss of teeth.
Effective treatment of periodontitis
The aim of the treatment is to eliminate the inflammatory condition of the gums and the supporting structures of the teeth, as well as to remove plaque, tartar, and pathogenic bacterial flora. Treatment is divided into different phases with various measures depending on the severity of the disease. In the so-called hygiene phase, all hard and soft deposits above the gum line are removed using PZR procedures. Several sessions may be necessary for this. Additionally, during this phase, dental and root fillings may need to be placed or renewed, and non-salvageable teeth removed. Even these hygiene measures alone can achieve noticeable improvement in many patients.
Subsequently, the "closed treatment phase" begins, during which the hard and soft deposits below the gum line are scraped away. This is done using specially shaped hand instruments and sonic and ultrasonic devices. After a healing period of 2 to 3 weeks, the outcome of this treatment is checked. If necessary, it is repeated in certain areas.
Gum pockets and periodontitis
In cases of very deep gum pockets (over 5 millimeters) that have not sufficiently receded through hygiene measures and closed treatment, it may be necessary to proceed to the open treatment phase. Under anesthesia, the diseased areas are surgically opened, the gums are folded back, and the inflamed bone and tooth areas are cleaned. The gums are then sutured microsurgically. Additionally, it is possible to fill cleaned bone pockets with bone substitute materials, cover with membranes, or stimulate regeneration with enamel matrix protein gel.
Modern regenerative periodontal therapy aims at the regeneration (new formation) of the periodontal tissue through surgical measures. These are procedures summarized under the term "guided tissue regeneration" (GTR). Damaged tissue can be regenerated through various methods, such as the use of bioactive bone substitute material, membrane technique, or growth proteins.
The 5 pathogenic, periodontal main bacteria are treated in different ways: For 3 types, curettage is sufficient, whereas for the other two, antibiotics must also be administered. Depending on the number of bone defects, these can be given in tablet form (systemically) or directly introduced into the gum pocket (locally). In both cases, it is advantageous to carry out a germ determination beforehand. However, it is pointless to treat the infection with antibiotics without cleaning the teeth first. Because the bacteria are almost completely protected in their biofilm from the effect of the antibiotic drug. Another local treatment method is the direct insertion of an antiseptic chlorhexidine chip into the gum pocket. This ensures long-term germ-free in the inflamed gum pocket and breaks down biologically by itself.
Prognosis
With timely and proper treatment, periodontitis can almost always be cured. However, this treatment is sometimes very long and always heavily dependent on the patient's cooperation. Every affected person must be aware that reinflammation is fundamentally possible. Therefore, even after the actual therapy has ended, regular follow-ups and professional teeth cleaning at 3-month intervals are necessary.
Exposed Tooth Necks / Recession Coverage / Gum Build-up
When individual tooth necks are exposed, this is usually the result of improper, too aggressive oral hygiene or improper loading of the teeth, for example, by grinding. Sometimes a poorly fitting Crown can be the cause. The gums retract on the outer surfaces of the teeth, making them appear longer. In addition, the affected teeth are often sensitive to hot/cold, and cavities can easily form on the exposed root.
Treatment of exposed tooth necks
After eliminating the causes of gum recession, the tooth necks can be covered again with micro-surgical techniques, either by shifting the surrounding gum or using a gum graft. As an autograft, a strip of gum is taken from the palate area. This is no more painful than a burn on the palate from eating a pizza that is too hot. The donor site on the palate heals after a week. When enamel matrix proteins (Emdogain) are also used, they enable true regeneration of lost gum. Emdogain consists of various proteins that combine to form a matrix and stimulate the formation of natural root cementum. Additionally, Emdogain has a positive effect on healing.
After the treatment
Initially, the affected area should not be cleaned with a toothbrush – it will be professionally cleaned during check-up appointments at the practice. Swelling may occur in the first three days, which subsides after about a week. Bruising is usually no longer visible after about 10 days. A light pain, which can be well managed with medication, is noticeable in the first few days following the procedure. Keeping the treated area cool also brings relief. When sleeping the head and upper body should be elevated. In the days following the treatment, exercise, physical exertion, smoking, caffeinated drinks, Alcohol as well as dairy products and grain-containing foods should be avoided. After recession coverage, a root coverage of an average of 90 percent can be achieved in the long term.
Risk factors for periodontitis (parodontosis)
Although the immune system and certain bacteria play the main role in the development of periodontitis, there are some risk factors that influence its development:
• poor or incorrect oral hygiene
• genetic predisposition
• tobacco consumption. Smokers have a 4 to 6 times higher risk of developing periodontitis compared to non-smokers.
• Diabetes mellitus (especially if the Blood sugar level poorly adjusted)
• Pregnancy. Hormonal changes cause connective tissue to loosen, gums to swell, and bacteria to invade.
• open dental caries
• Mouth breathing
• Bruxism (mostly stress-related Teeth grinding)
• unbalanced diet
Connection between periodontitis and diabetes
Periodontitis affects systemic diseases such as diabetes or chronic cardiovascular diseases. A connection between periodontitis and the vascular disease arthritis is also discussed. Studies have demonstrated a link between gum disease and the increased risk of premature births (or newborns with below-average birth weight): It is almost eight times higher than in women with healthy teeth and gums.
Risks of periodontitis treatment
As with any surgery, there is a risk of wound infection. Mild pain, swelling, and minimal bleeding are normal until the third day.
After periodontitis treatment
After the local anesthesia wears off, patients usually feel a slight pull in the treated area. For the period after the treatment, the doctor prescribes anti-inflammatory painkillers, an antibacterial mouthwash with chlorhexidine, and possibly antibiotics for 5 to 8 days. Slight swelling and bruising may occur until the third day. Brushing your teeth in the treated area should be avoided. It is normal for the wound to bleed slightly during the first few days. Patients should keep their head elevated while sleeping. The stitches will be removed after 8 to 10 days.
Other Treatment Methods in this Department
Experts for this Treatment Method

- Aesthetics & Function in Dentistry
Dr. Dr. Ákos Fehér
Fehér Dental Team, Smile Lounge
- Aesthetics & Function in Dentistry
Dr. med. dent. Malte Schönrock M.Sc., M.Sc.
Dent Aesthetic
- Aesthetics & Function in Dentistry
Jan Kurtz-Hoffmann
Zahnärzte im Roßbachpalais
- Aesthetics & Function in Dentistry
Dr. med. dent. Tore Thomsen
Zahnarztpraxis Dres. Thomsen & Kollegen
- Aesthetics & Function in Dentistry
Dr. med. dent. Oliver Brendel
Dinkelacker & Brendel
- Aesthetics & Function in Dentistry
Zahnarzt Robert Svoboda M.Sc.
ZahnGesundheit OberkasselAll Experts in this Department
Show All
- Aesthetics & Function in Dentistry
Dr. Dr. Ákos Fehér
Fehér Dental Team, Smile Lounge
- Aesthetics & Function in Dentistry
Dr. med. dent. Malte Schönrock M.Sc., M.Sc.
Dent Aesthetic
- Aesthetics & Function in Dentistry
Jan Kurtz-Hoffmann
Zahnärzte im Roßbachpalais
- Aesthetics & Function in Dentistry
Dr. med. dent. Tore Thomsen
Zahnarztpraxis Dres. Thomsen & Kollegen
- Aesthetics & Function in Dentistry
Dr. med. dent. Oliver Brendel
Dinkelacker & Brendel
- Aesthetics & Function in Dentistry