Other Treatment Methods
- Adrenal hyperplasia
- Gestational diabetes
- Growth disorders in children
- Hashimoto's thyroiditis
- Hormone deficiency
- Hormone-producing tumors
- Hyperthyroidism
- Hypofunction of the adrenal cortex
- Hypothyroidism
- MODY (Maturity Onset Diabetes of the Young)
- Obesity
- Osteoporosis
- Overactivity of the adrenal cortex
- Sex hormones
- Type 1 diabetes
- Type 2 diabetes

© Freepik
Hashimoto's thyroiditis
Hashimoto's thyroiditis (inflammation of the thyroid gland) is the most common cause of an underactive thyroid hypothyroidism and is considered one of the autoimmune diseases. In this condition, the body’s immune system attacks and slowly destroys the thyroid cells, which leads to a reduced production of hormones in the long term. The disease predominantly affects women, mostly in middle age, but can also occur in men, adolescents, or children. The cause is a misguided immune reaction where antibodies are formed against components of the thyroid gland. Why this autoimmune reaction occurs is not completely understood, but genetic predisposition, hormonal changes (such as during pregnancy), environmental factors like excessive iodine intake, or viral infections are considered possible triggers.
The symptoms develop slowly and are often recognized late. Initially, there may be a temporary hyperthyroidism because inflamed thyroid cells release their stored hormones. In this phase, symptoms such as rapid heartbeat, nervousness, or weight loss occur. However, as the condition progresses, a permanent hypothyroidism develops. Typical complaints here include fatigue, listlessness, weight gain, sensitivity to cold, concentration difficulties, dry skin, hair loss, and an enlarged or hardened thyroid gland. Fatigue, listlessness, weight gain, sensitivity to cold, concentration difficulties, dry skin, hair loss, and an enlarged or hardened thyroid gland.
Diagnosis of Hashimoto's thyroiditis
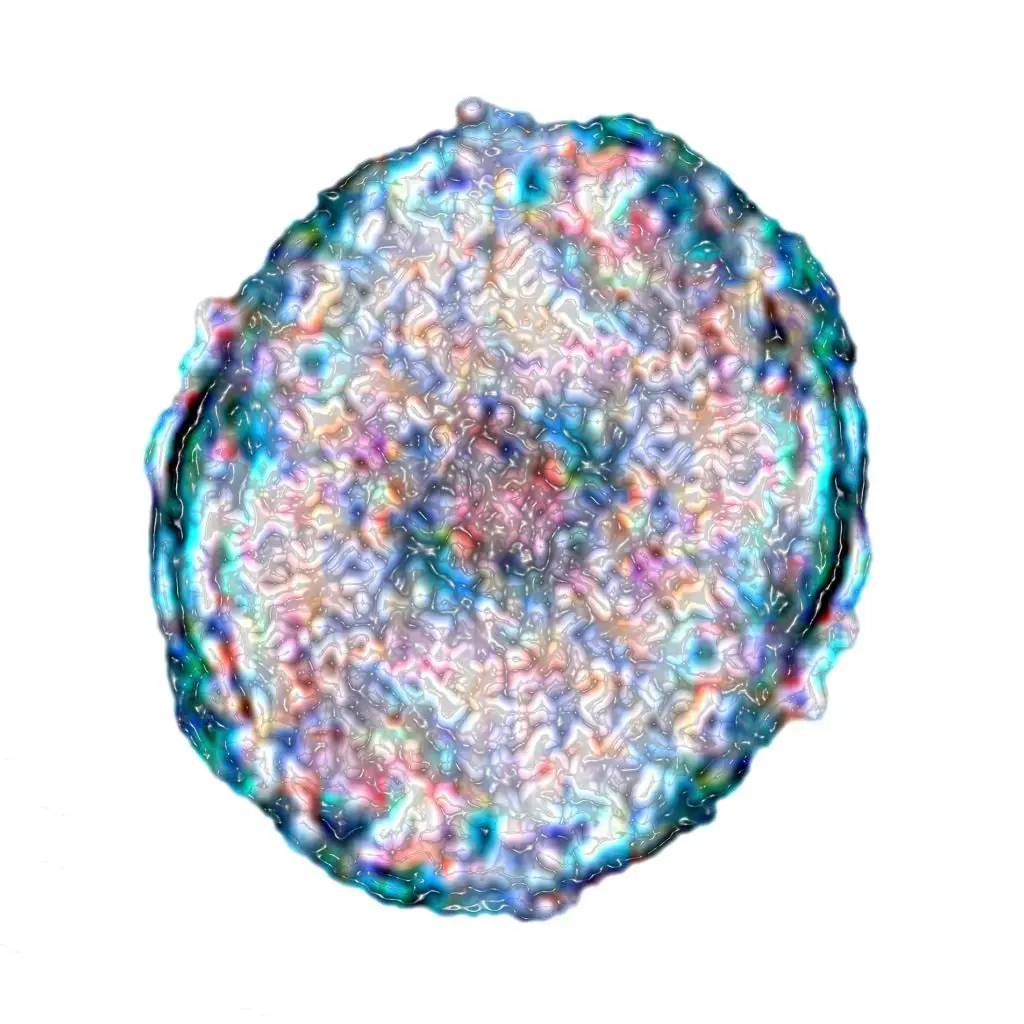
The diagnosis is made through a combination of laboratory values and ultrasound examination. The blood often shows an elevated TSH level as an indication of hypothyroidism, decreased free thyroid hormones (fT3, fT4), and the presence of specific autoantibodies. In the ultrasound image, the thyroid often appears inhomogeneous, hypoechoic – that is, very dark – and reduced in size.
Treatment of Hashimoto's thyroiditis
The therapy depends on the severity of the hypothyroidism. Usually, a lifelong substitution therapy with a synthetic thyroid hormone is carried out to compensate for the hormone deficiency. The dosage is individually adjusted based on TSH levels and symptoms. A special diet or alternative measures can anti-inflammatory act, but do not replace hormone administration. Regular medical supervision is essential, as hormone levels can change throughout life. The aim of the therapy is to establish a normal metabolic state and ensure the quality of life for those affected.