One year after the last menstrual period, the final phase of menopause begins: postmenopause (post = Latin for after). From now on, it becomes noticeable how the fluctuations in hormone levels, particularly progesterone and estrogen, gradually decrease – and as a result, menopausal symptoms also become less severe.
When does postmenopause begin and how long does it last?
Menopause (and thus also postmenopause) is determined retrospectively, not predicted. It is considered confirmed when the last menstrual period was more than 12 months ago. On average, this occurs at the age of about 51 or 52 years.
Postmenopause extends over a period of ten to 15 years, with the first five of these also being referred to as early postmenopause. Between the ages of 60 and 65, the so-called senium follows postmenopause.
Postmenopause: Symptoms at the end of menopause
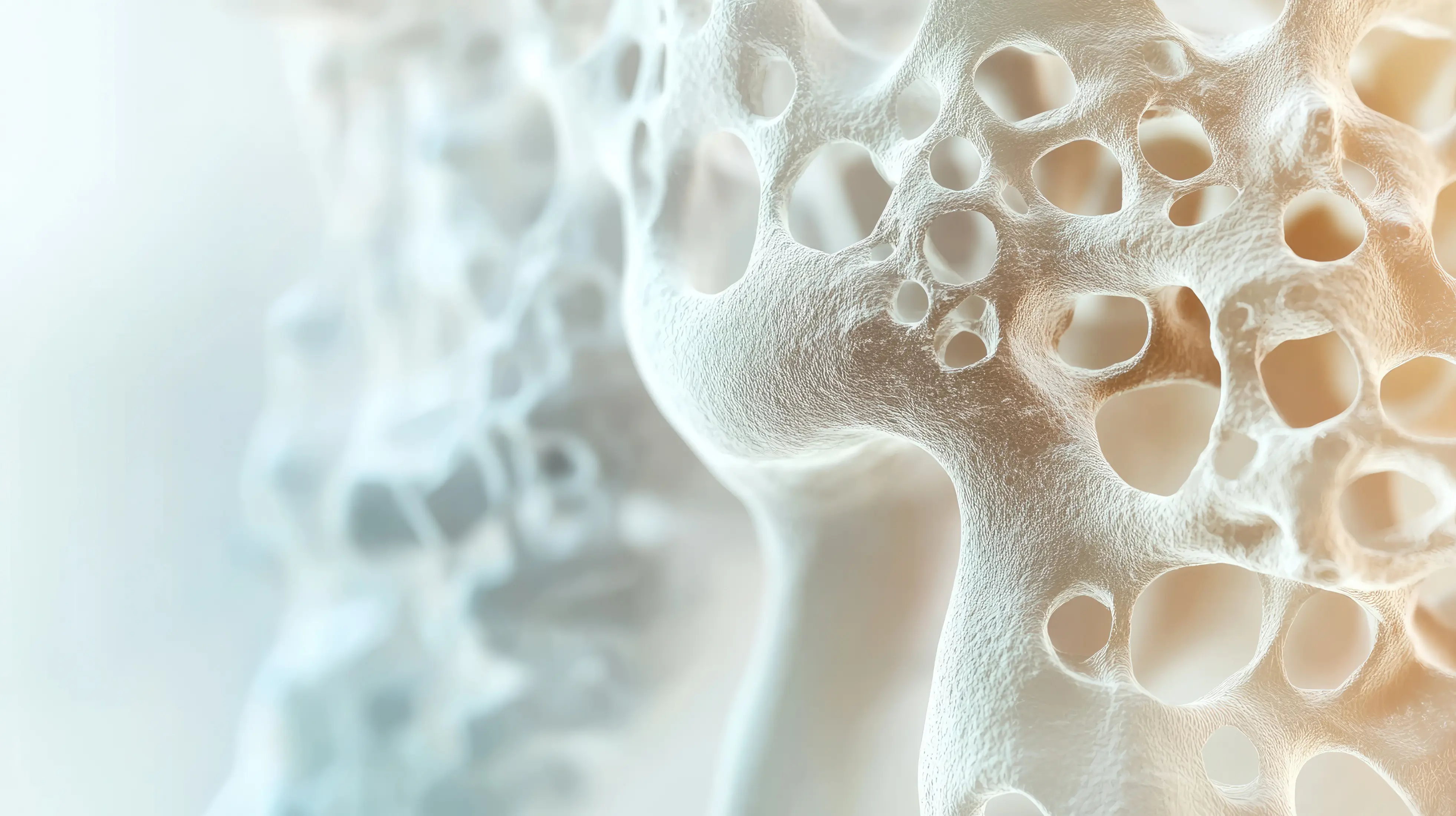
Particularly common during postmenopause are complaints such as back and joint pain and dry skin. In this phase of life, many women are particularly prone to developing osteoporosis.
The symptoms during postmenopause are often similar to those from previous phases of menopause. Typical now are:
- Sleep disorders
- Hair loss
- Hot flashes
- Depressive mood
- Weight gain
- Dizziness
- Loss of libido
- Dry skin
Hormonal imbalance during postmenopause - the risk for diseases increases
Since the production of estrogen drops drastically during menopause - and hardly takes place at all in the end - but the amount of testosterone (male sex hormone) changes little, a hormonal imbalance occurs, which can lead to "masculinization phenomena." For example, hair loss, but at the same time, increased facial hair growth ("lady's beard").
Skin problems in postmenopause
Estrogens are involved in the retention of fluid in cellular tissue. If they are missing, the skin becomes less elastic and drier, leading to the formation of wrinkles. It is therefore important to support the skin at least externally with sufficient moisture in the form of creams. An increasing pigment deposition also increases the likelihood of age spots.










_1500x2250_150_RGB-2.webp)